Annual Report and Accounts 2024-25
Date published: 19 August 2025
Summary
Our annual report is produced so that we can present information about our services and report on our performance. We do this in line with our commitment to openness and transparency and the published guidance set out by the Department for Health and Social Care (DHSC).
In this report
- Introduction
- Welcome from the chair
- Overview from the chief executive
- Compliments and complaints
- About EEAST
- Highlights from 2024-25
- Section 1 - Be an exceptional place to work, volunteer and learn
- Our People
- Staff Experience
- Our volunteers
- Section 2 - Provide outstanding quality of care and performance to our patients
- Patient safety
- Non-Emergency Patient Transport Services
- Section 3: Delivering outstanding care, with exceptional people, every hour of every day
- Urgent and Emergency Services
- Call Pick Up
- Hear and Treat
- Organisational Performance Improvement Plan (OPIP)
- Out of Service
- Hospital Handover
- Resilience and specialist operations
- Digital Development
- Section 4: Be excellent collaborators and innovators as system partners
- Commercial partnerships
- Section 5: Be an environmentally and financially sustainable organisation
- Sustainability
- Carbon Footprint
- Resource Optimisation
- Task Force on Climate-related Financial Disclosures (TCFD)
- Section 6: Delivering our strategic goals
- Developing the strategy
- The EEAST Strategic Framework
- Continuous Evolution
- Section 7: Accountability report
- Directors Report
- Annual Governance Statement
Introduction
Welcome from the chair
One of the best things about being on the board of EEAST is having the opportunity be out and about to meet staff and patients. I thought I would start this year’s report with a couple of stories from the board about what we saw and heard from you over the year.
I joined a crew who collected a patient from hospital to take him to a hospice. As we sat and talked in the back of the ambulance, I realised that the EEAST staff had the enormous responsibility of caring for this gentleman on what would probably be the last journey he would ever make. At the other end of the scale, one of my board colleagues was with a crew as they were called out to a woman in labour, and he had the privilege of being present as a new life was safely brought into the world by EEAST staff.
These stories (and everything in between) sum up what it is like to be part of EEAST, and they frame my reflections on our work over the last year.
Firstly, our staff and their experience of working at EEAST are paramount to us as a board and in this report, we share some of the work we have been doing to improve our staff welfare and culture. Our flagship programme, “Time to Lead” aims to give our managers the skills and capacity to address what has historically been an area of great concern. We are delivering great results with staff turnover and sickness levels reducing. Also, our staff are telling us they are feeling the benefit – I am immensely proud that EEAST is again the most improved ambulance trust for the third year running in the NHS staff survey.
However, whilst what we are doing is working, we still have a long way to go. I am only too aware of incidents of bullying and harassment, including concerns about sexual safety which have been a part of the culture here at EEAST for too long. I and the entire board are determined to drive these behaviours out and call for everyone’s help to do this.
The second area of board focus has been our response times to patients. Over the last year, we have analysed our performance data to ensure we use our resources in the most effective way. The result is our Operational Performance Improvement Plan (OPIP) described later in this report. The impact of this is clear to see with notable improvements in our category 2 performance in quarter 4 despite longer hospital handovers. Again, whilst we are confident that our plans are working, our response times are still too slow, and we have plans to make even greater improvements over the coming year.
Which brings me to the third area of priority for the board, partnering with our colleagues across the health and care sectors. There are many examples that I could highlight - like our work with acute hospitals to manage handover delays; our mental health response units that regularly achieve an 85% non-conveyance rate; and the continued growth of our unscheduled care hubs in each of our six partner Integrated Care Systems.
We have also developed our new 2025-30 strategy and values. I am proud to say, this was heavily co-produced with our staff, patients and partners with literally thousands of touch points as we developed our thinking. The next stage for the board is to build the multi-year business plans that will deliver it. Co-production was also key in the recruitment of Neill Moloney as our new Chief Executive. We engaged with staff and stakeholders at every stage from input into the job description to the final interview. Neill replaced Tom Abell who had led EEAST as Chief Executive for 3 years – I’d like to take this opportunity to thank Tom for his hard work and the strong foundations he left us with.
Neill and our strategy will be tested over the next year. It is apparent that the pace of change in the public sector and the NHS is not likely to abate and if anything will accelerate. The next year is going to be busy, but I also believe it will be one of great progress and opportunity. EEAST is well positioned to succeed in what will be a greatly changed health and social care environment.
Finally, I would like to take a moment to thank the many people who have helped and supported me, the board and the organisation over the course of the last year. I have had the pleasure of being out and about and meeting many members of staff, volunteers, community representatives and patients. Thank you for taking the time to talk to me and share your thoughts and experiences – I have learnt something from every conversation.
Mrunal Sisodia Trust Chair, OBE.
Overview from the chief executive
At the East of England Ambulance Service NHS Trust (EEAST) our unwavering commitment to patient care and staff wellbeing drives every aspect of our operation. We strive to deliver an outstanding service whenever and wherever our patients need it, and to enable and empower our people to work in an organisation which is inclusive, responsive to their wellbeing needs and fosters a culture of excellence. Reflecting on the last year, we recognise the challenges we have faced, and the improvements delivered with the support of our staff, communities and regulators.
We continue to work to reduce our C2 response times to ensure our patients receive the right care, at the right time. We have implemented a range of strategies to support this, such as increasing our collaboration with community providers to support patients to access alternative sources of care, where clinically appropriate through the urgent and emergency care hubs in all counties in partnership with the ICBs.
I’m particularly proud of the unscheduled care co-ordination hub in Norfolk and Waveney 62% of their calls from the stack since its launch in September 2023, avoiding unnecessary ambulance responses while improving patient outcomes and system efficiency. In 2024, 46,864 calls were passed via our Access to the Stack process across the Trust.
The single biggest contributor to C2 response times is hospital handover delays. In November 2024 the Trust launched ‘Handover 45' with the support of commissioners and acute Trusts. The primary aim is to reduce avoidable harm, in communities because of delayed ambulance response times, which are consequential to delayed handovers of emergency patients at acute trusts. Where handover of patients from the ambulance service to hospitals in 45 minutes has been delivered consistently, avoidable harm has demonstrably reduced.
The Trust continues to deliver on its cultural change journey to support and improve the wellbeing of our people. In the last year, we have restructured our operational directorate to ensure the spans of control for any single manager have reduced to a level which enables them to meet the needs and support requirements of the staff they are responsible for.
We have also launched a new 24-hour, 365 day a year Freedom to Speak Up Service to enable our staff to feel confident to speak up and raise their concerns in a safe, independent, resilient and confidential space. We have enhanced our wellbeing offering with the launch of the Time For Me app to support our staff to pro-actively manage both their mental and physical health and we have also implemented wellbeing rooms across the Trust. These changes are just one step in ensuring our people are working in an organisation in which they feel supported and empowered by an organisation which listens to their concerns and acts on their feedback.
The annual NHS staff survey showed more staff reporting that they felt they could report experiences of harassment, bullying or abuse following the speak out campaign, staff reporting they had not experienced discrimination from patients and service users and more staff reported there were enough staff to do their job properly which improved following a drive in recruitment across clinical operations. We recognise there is more to do, and we are committed to our journey to excellence.
Over the past year, EEAST’s commercial services made significant progress in aligning business units under a unified commercial strategy, focusing on revenue generation, service diversification, and the delivery of measurable social value.
Commercial growth continued to accelerate, and their financial contribution exceeded the initial forecasts. This was reinvested by EEAST to enhance patient care and community health outcomes.
As we move into the next year, our commitment to enhancing patient outcomes and fostering a culture of excellence remains steadfast. These improvements would not be possible without the support of our people, volunteers, partners and communities. We are committed to maintaining the highest standards of care for our communities as an organisation which acts with unwavering integrity, and a workforce which is accountable, respectful, and strives to be excellent.
Neill Moloney, Chief Executive Officer
Compliments and complaints
Most people were generally happy with the service they received (as evidenced by the high ratio of compliments to complaints received, and most patients reporting satisfaction on their friends and family test). Where people were unhappy with the service they received, they often felt that improvements could be made around communication or timeliness. Below is a selection of patient quotes which are representative of much of the feedback received over the year.
Compliments:
-
"The crew were professional, caring, very friendly and put me at ease. They provided me with re-assurance in a stressful time.” (Emergency and Urgent Care).
-
“The crew were punctual professional and very friendly. They went above and beyond to ensure I got home safely.” (Patient Transport Service).
-
“I was very impressed by the two paramedics who attended me when I was feeling very unwell. They performed a full range of tests and found it unnecessary for me to go to hospital and that I could be treated at home. They were very informative to me and my son/carer.” (Emergency and Urgent Care).
-
“The ambulance service responded immediately, the expertise my wife experienced from your crew was exemplary with compassion” (Emergency and Urgent Care).
-
“The ambulance crew that took me to and from my home to hospital were so lovely, very patient, they made me feel at ease. Very professional throughout and made the journey completely stress free' (Patient Transport Service).
-
“The call handler was very calm and helpful, they stayed on the line until the paramedics arrived in our house which was really good, thank you” (Emergency and Urgent Care).
Complaints:
-
“One was very kind and helpful, but the other spoke to me like I was 5 years old telling me off for wasting her time." (Emergency and Urgent Care).
-
“Received a phone call 3 hours later saying ambulance will not come anymore and I should call GP in the morning.” (Emergency and Urgent Care).
-
“I was very disappointed by the lack of communication; I was not even called or informed that the Patient Transport are running late" (Patient Transport Service).
About EEAST
The East of England Ambulance Service (EEAST) provides emergency and urgent care services throughout Bedfordshire, Cambridgeshire, Essex, Hertfordshire, Norfolk and Suffolk.
The east of England is made up of both urban and rural areas with a diverse population. As well as a resident population of about 6.3 million people, several thousand more tourists enjoy visiting our area in peak seasons each year. Our area also contains several airports including London Luton and London Stansted as well as major transport routes which increase the number of people in our region daily.
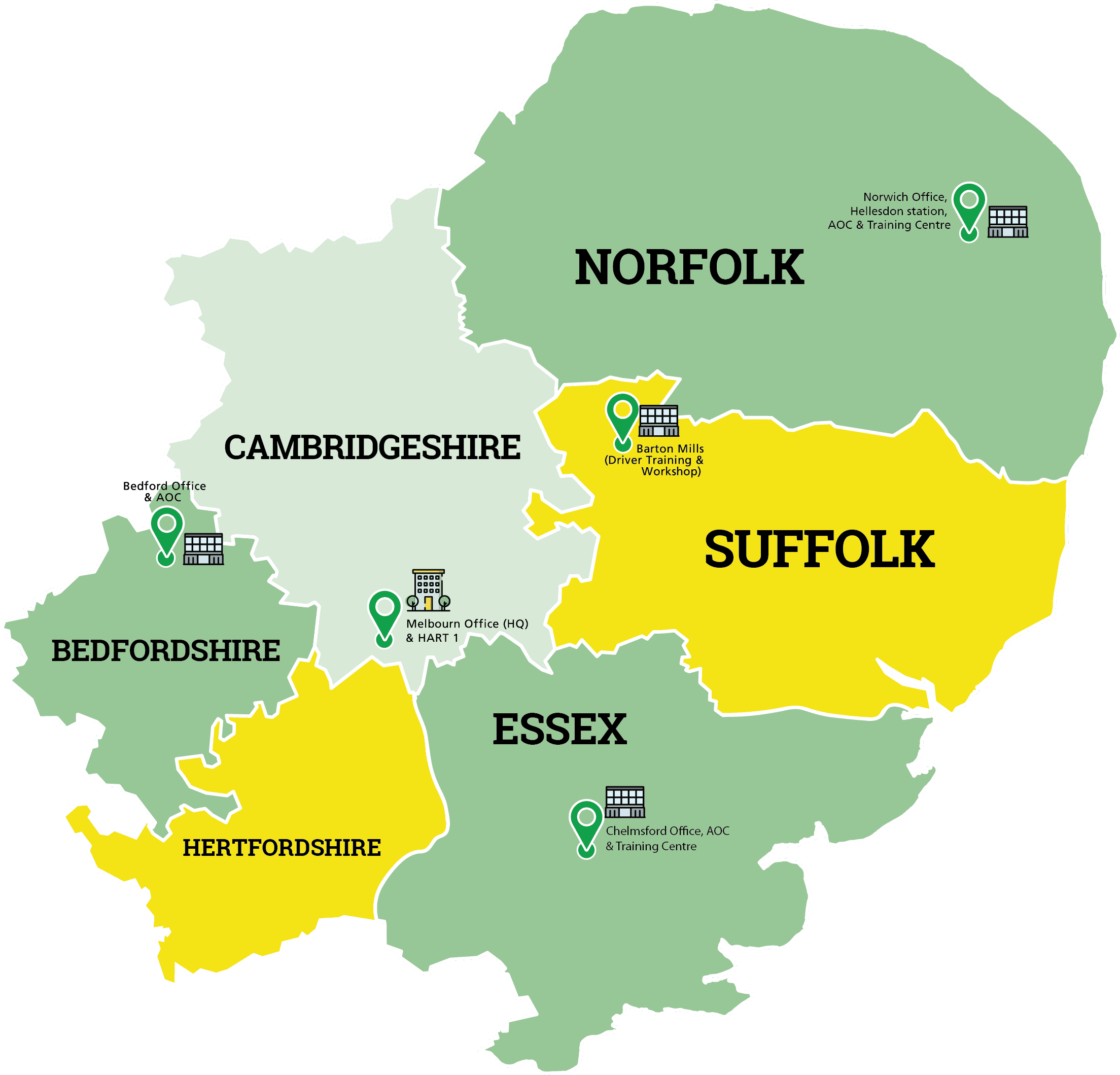
During 2024/25 we provided non-emergency patient transport services for patients needing non-emergency transport to and from hospital, treatment centres and other similar facilities within Cambridgeshire, parts of Essex, Bedfordshire and Hertfordshire.
We work with six Integrated Care Systems (ICS) covering an area of approximately 7,500 square miles.
We employ more than 6,000 colleagues operating from over 120 sites and are supported by more than 1,500 dedicated volunteers working in a variety of roles including: Community first responders; volunteer car drivers; BASICS doctors; chaplains and our community engagement group.
EEAST’s Headquarters is based in Melbourn, Cambridgeshire and there are ambulance emergency operations centres (EOC) at each of the three locality offices in Bedford, Chelmsford and Norwich which receive over 1.3 million emergency calls from across the region each year as well as calls for patients booking non-emergency transport.
Response to 999 calls as an emergency and urgent care service
IIn 2024/25, our emergency operations centre (EOC) received 1,384,547 emergency contacts from the public.
On average, over 2,750 emergency 999 calls came into the ambulance service every day.
Call handlers record information about the nature of the patient’s illness or injury using sophisticated software to make sure they get the right kind of medical help. This is known as triaging and allows us to ensure that the most seriously ill patients can be prioritised and get the fastest and most appropriate response.
Scheduled care service – Patient Transport Service (PTS)
We deliver a Non-Emergency Patient Transport Service (NEPTS), working in collaboration with hospitals and treatment centres, transporting and caring for a variety of patients, including elderly and vulnerable people, and those with mental ill health, to and from outpatient clinics, day-care centres, and other treatment facilities.
Colleagues are trained to lift and manoeuvre patients in and out of vehicles, ensuring patients are safe and comfortable during the journey and arrive on time for appointments. Colleagues are trained to administer first aid or life-saving techniques should this be necessary. Other duties include making sure vehicles are clean and tidy, in line with strict infection and prevention guidelines and keeping accurate records of journeys.
During 2024/25 we undertook 437,647 patient journeys and 41,728 escort journeys – a total of 479,375 NEPTS journeys.
Resilience and special operations
EEAST operates two hazardous area response teams (HART) and has a resilience and specialist operations team which oversees the Trust’s preparation for responding to a major incident along with business continuity incidents. The team works very closely with partner agencies and local resilience forums.
Commercial services
We operate several commercial services that generate income for the Trust, as well as providing organisational resilience.
CallEEAST, our non-emergency and commercial contact centre, offers an array of contact centre solutions to commercial organisations and other NHS Trusts.
The team supports 80 separate contracts handling more than 850,000 calls every year.
The National Performance Advisory Group (NPAG) brings people together nationally to share best practice and showcase industry developments across the NHS enabling innovation and efficiency.
TrainEEAST, EEAST’s commercial training department offers a wide range of first aid and emergency care training courses for businesses, organisations, individuals and our own colleagues.
Finance
During the financial year 2024/25 EEAST spent £496.5m, an increase of £54.5m over the previous year 2023/24. There was also an increase in income received of £55.5m to £498.4m (2023/24 £442.9m) which generated a surplus for the year of £1.9m (2023/24 £0.9m). The original financial plan for 2024/25 was to deliver a break-even position.
The income arrangement with our commissioners continued to be via a ‘block’ income arrangement. The most significant financial change for 2024/25 was the £18.7m full year impact of the investment from the national Urgent and Emergency Care (UEC) funding (2023/24 £12.5m, total recurrent funding £31.2m), to support national ambulance priority areas such as C2 response and hear and treat.
We continued to focus on cost efficiency targets across 2024/25. £16.3m was achieved against our target of £16.2m, although a significant element was on a non-recurrent basis. The cost efficiency target for 2025/26 is planned at £14.9m. Activity is underway to deliver primarily recurrent efficiencies to this value, with a restructuring provision of £1.6m in the 2024/25 accounts to enable this.
The Board will continue to monitor our financial position and key risks.
EEAST has submitted a draft plan for 2025/26 which is based on a balanced budget.
Across 2024/25 EEAST invested £25.0m in capital assets:
- £17.9m invested in building projects, including the new Ipswich Hub, £9.5m of which has been funded by DHSC public dividend capital. Other projects included expansion and reconfiguration of Hellesdon EOC and development and refurbishment of other existing sites.
- £3.3m was invested in new vehicles and vehicle equipment, including replacement of HART vehicles and mental health vehicles.
- £2.1m was invested in medical devices such as Corpuls.
- £1.7m investment in IT for the electronic patient care record (ePCR), connectivity and cybersecurity projects.
- Disposals reflect the previously capitalised Ambulances for sale and leaseback.
The full financial statements for the year ending 31 March 2025, are presented within the Annual Accounts.
Highlights from 2024-25
April 2024
Paramedics met up with a mother and her baby a year after they assisted with a dramatic birth in the car park of Chelmsford ambulance station.
May 2024
The Defence Employer Recognition Scheme (DERS) re-accredited EEAST with the Gold Award for a further five years for its support for the defence and Armed Forces community.
June 2024
Volunteer community first responder, Nathan Liberman was recognised for his 17 years of service to the NHS and the north Norfolk community in the King’s Birthday Honours.
July 2024
We welcomed students with autism from Wherry School in Norwich for a work experience placement for the second year running.
August 2024
Shortlisted for the HSJ Awards in the Provider Collaboration of the Year category, for our partnership with regional fire and rescue services in assisting people who have fallen at home.
September 2024
Robert Rous, Vice Lord-Lieutenant of Suffolk officially opened our new multi-million-pound ambulance hub in Bury St Edmunds - the most sustainable and lowest carbon site in the Trust’s estate.
October 2024
Essex’s first female paramedic, Sally Pattie retired after 44 years with East of England Ambulance Service NHS Trust.
November 2024
Awarded the Inclusive Workplace Award at the British Dyslexia Association Annual Award.
December 2024
Staff from our Emergency Operations Centres in Norwich and Chelmsford donated over 1,000 gifts to the Salvation Army Christmas Present Appeal.
January 2025
New partnership launched with trained firefighters at London Luton Airport (LLA) to respond to the most serious medical emergencies within the airport boundary.
February 2025
A new community defibrillator was installed at a fire station in Royston, in dedication to Rod Taylor, a long-serving paramedic who managed community defibrillators.
March 2025
Awarded a four-year-old girl from Suffolk a bravery award for calling 999 when her mum became unresponsive at home.
Our People
Central to our vision is the steadfast belief that EEAST should not only be a place to work but a community where individuals feel valued, supported, and inspired. We recognise that our success hinges on the wellbeing, engagement, and professional development of everyone within the organisation. Throughout 2024/25, we focused on building a culture that prioritises openness, inclusivity, and collaboration.
Our cultural improvement journey continued to progress throughout 2024/25, with concerted efforts to cultivate an environment that promoted learning, growth, and collaboration. We worked to empower our workforce by enhancing communication channels, providing more accessible leadership support, and fostering a culture of openness. The emphasis was on creating a supportive environment where all staff feel confident and equipped to deliver high-quality care, knowing their contributions are recognised and valued.
A significant part of our cultural journey involved evolving our values. Last year, we began the process of refining our core values, moving from five previous values to three new, clearer values. Over 1,000 colleagues were involved in designing them, and these new values were tested with over 100 colleagues through workshops in November. The result is a more streamlined and actionable set of values:
- We are Accountable
- We are Respectful
- We strive to be Excellent
These values are not only at the heart of our culture but also serve as guiding principles in how we work, interact, and grow together. We are integrating these values into all aspects of our organisation, from how we present them to staff to how they are used in appraisals and beyond. We employ 6,539 people, 55.45% of our workforce are female and 6.4% of our staff are black or minority ethnic.
Our workforce is made up of 735 people working in support services, 4,173 in accident and emergency operations, 776 in emergency operations centres, 365 in patient transport services, 320 in operational support and estates and 170 in air and special operations.
People Strategy
Our People Strategy was focused on strengthening partnerships, improving communication, and enhancing staff engagement through a series of targeted initiatives. Central to this strategy was a three-year action plan designed to align organisational development with the evolving needs of our workforce.
To support this, we introduced a fixed-term people promise manager role, tasked with overseeing the implementation of the NHS people promise pillars across EEAST. This role was instrumental in fostering collaboration across all levels of the organisation, aiming to improve the experience of working within the NHS. Since July 2024, the people promise manager engaged in over 1,300 staff contacts, reflecting our ongoing commitment to employee engagement. In addition, a new peer-to-peer recognition platform was developed to help embed a culture of appreciation across the organisation. As part of our involvement in the national people promise exemplar programme, EEAST developed a comprehensive plan for staff reward and recognition.
Significant progress was made in recognising long service. A new booking process was shared with eligible staff, and six award ceremonies took place during March 2025. A formal proposal for the future approach to long-service recognition has been submitted for consideration by EEAST’s Executive Team. Policy development was another area of focus, with revisions to key documents including occupational health, disability and long-term health conditions, professional registrations, and annual leave policies. These updated, published in February 2025, are intended to improve clarity, consistency, and accessibility for all staff.
Our employee engagement efforts have been further enhanced through initiatives such as Emergency Operations Centre (EOC) celebration days, focus groups to support EOC retention, and a comprehensive update to the pensions and retirement intranet pages. Additionally, EEAST introduced a reasonable adjustments advisor role and process to provide better support for staff requiring workplace adjustments.
We successfully completed our year two actions and commenced the longer-term initiatives scheduled for 2024/25 and 2025/26. As we approach the final year of our current people strategy, preparations are underway to review and refresh our strategic priorities moving forward.
We have launched the Green Network and now have 43 Green Champions.
Recruitment and Retention
Between April 2024 and March 2025, EEAST recruited 684 individuals, primarily into frontline roles. This contributed to achieving 3,572 whole time equivalent (WTE) staff within our clinical workforce plan, against a target of 3,587 WTE.
The average time to hire during this period was 12 weeks, compared to a target of 12 weeks.
Course fill rates averaged 82.5%, falling slightly below our target of 85%.
Looking ahead, recruitment efforts will focus on expanding our apprenticeship pathways, with a particular emphasis on training emergency care assistants (ECAs) internally. Additionally, targeted recruitment will continue to address vacancies within our emergency operations centres (EOCs), especially for call handler roles. To enhance the onboarding experience for new starters, we will be launching a digital corporate induction. This development aims to provide a consistent, engaging, and accessible introduction to EEAST for all new employees.
Our ‘career for life’ campaign continued throughout 2024/25, featuring online workshops and Q&A sessions for prospective applicants. Feedback from attendees was overwhelmingly positive, indicating strong engagement and interest in EEAST as an employer of choice.
Recruitment processes were further streamlined during the year to reduce delays and improve the candidate experience. A key priority was to increase the diversity of our workforce. Guided by the EEAST inclusivity plan, our recruitment strategies aimed to attract candidates from underrepresented groups. As a result, we achieved 6.44% representation against a target of 7%.
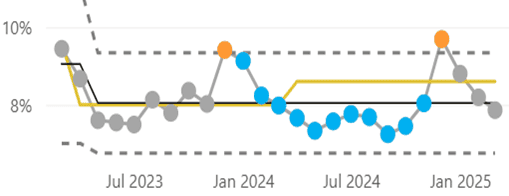
Retention and turnover remained critical challenges across the NHS. EEAST’s turnover rate improved steadily, decreasing from 8.74% in April 2024 to 8.44% in March 2025. This positive trend reflects the impact of sustained long-term interventions focused on retention.
Key retention initiatives include:
- Strengthening career progression pathways
- Enhancing leadership development programmes
- Expanding mentoring opportunities
- Improving internal communications to ensure staff feel heard and supported.
Feedback from exit questionnaires, stay at EEAST conversations, and focus groups informed targeted action plans to address specific retention concerns, led by our HR Business Partner (HRBP) Team.
Flexible working arrangements and enhanced wellbeing resources continued to be promoted as part of our broader commitment to supporting staff wellbeing and work-life balance.
We were proud to be recognised for our commitment to inclusivity by the British dyslexia association, receiving the inclusive workplace award at its annual awards in 2024. This honour acknowledged our pioneering efforts in creating a neurodiverse-friendly environment and supporting staff with dyslexia. In September 2024, we became the first NHS organisation and emergency service to achieve the silver quality mark, and we are now working towards achieving the gold standard.
During 2024/25, our enhanced redeployment process successfully retained 28 individuals, ensuring valuable skills and experience remained within the organisation. Looking ahead to 2025/26, we will be introducing team based working, building on the foundations of the time to lead change programme. This initiative was designed to reduce leadership spans of control, promote people-focused leadership, and ensure all frontline staff are supported within clearly defined team structures.
Staff Survey and Staff Experience
The National Staff Survey remained a crucial tool for understanding the experiences, perceptions, and concerns of our workforce. During 2024/25, EEAST achieved a significantly higher response rate than in previous years, reflecting increased staff engagement and a growing culture of feedback. Fieldwork was conducted during October and November 2024, with participation from nearly 50% of our workforce.
Survey results were communicated transparently across the organisation and informed the development of tailored, local action plans focused on key improvement areas such as communication, workload management, and professional development. EEAST maintained its position as the top-performing Trust for the third consecutive year in terms of overall improvement across all survey questions.
In recognition of this sustained progress, EEAST received a certificate from NHS England, acknowledging consistent improvement across all seven NHS people promise elements, as well as the key themes of staff engagement and morale, over two consecutive years.
In addition to the national staff survey, staff experience was continually measured through regular feedback mechanisms, including pulse surveys, focus groups, and engagement forums. This ongoing dialogue ensured that staff feel heard, valued, and involved in shaping the working environment.
Our commitment to meaningful engagement was further supported by our staff networks and sector-level change networks, which played a central role in creating inclusive, responsive forums for staff voice. These activities were a core part of our broader culture-based work, which integrated a range of initiatives aimed at improving and sustaining a positive organisational culture. Progress was actively measured and monitored to ensure long-term impact.
Notably, 97% of responses in the most recent survey either remained consistent or showed improvement compared to the previous year—underscoring the effectiveness of our people-centred approach.
In line with our commitment to supporting all staff communities, we are launching a new armed services network during 2025/26. This initiative will enhance support for our many colleagues with military backgrounds and reinforce our responsibilities as a veterans’ aware employer.
Appraisal and Leadership Development
We are committed to fostering a culture of continuous growth, meaningful feedback, and strong leadership. During 2024/25, we continued to strengthen our appraisal process to ensure it was supportive, consistent, and aligned with both individual and organisational objectives. Clear guidance and toolkits were provided to managers to support preparation and promote a fair, structured approach to performance conversations.
A key milestone last year was the completion rate of 87% for annual appraisals—a significant step toward our goal of ensuring every member of staff receives regular, quality feedback and development planning. To support this, we introduced the Staff Circle platform, a simple and user-friendly system designed to facilitate more meaningful and compassionate conversations. It also enabled improved tracking of appraisal completion, objective setting, and personal development planning.
In future, it will support us in identifying workforce-wide training needs and ensuring development opportunities are relevant and impactful. To promote consistency and values-based reflection, we also introduced a values self-assessment framework. This tool encouraged staff to align their behaviours and development goals with EEAST's core values.
Leadership development remained a cornerstone of our people strategy. During 2024/25, we expanded our leadership development framework—a structured programme designed to equip leaders with the skills to lead with confidence, empathy, and inclusivity. Training included mental health awareness, inclusive leadership, and conflict resolution.
By March 2025, 67% of our senior leaders at a Band 7 and above had participated in phase 1 of the programme. Phase 2 is now being delivered locally to newly appointed team leaders, as well as to leaders across support services, emergency operations centres, and corporate services. Executive directors are scheduled to begin their sessions in June 2025, with Phase 3 of the framework planned for launch later in the year.
In support of compliance and statutory responsibilities, a focused campaign in targeted improvements in statutory and mandatory eLearning. This initiative has already resulted in a measurable uplift in compliance rates which stands at 93.53%.
As part of the continuous evolution of our appraisal process, we will be launching training from April 2025 to support leaders in conducting effective, high-quality appraisal conversations. This training aims to further embed compassionate leadership and ensure every conversation contributes positively to the employee experience and professional development.
We believe that working with us is more than a job—it’s a career for life. Through our ongoing investment in leadership and development, we aim to ensure all staff are supported to thrive, grow, and fulfil their potential.
Safety at Work
Creating a safe, supportive, and inclusive working environment remained a top priority for EEAST. Throughout 2024/25, we implemented a range of initiatives aimed at improving both psychological and physical safety for our workforce.
A key development was the introduction of the managing stress at work policy, accompanied by practical risk assessment templates to support teams in identifying and mitigating work-related stress. Additionally, our welfare wagons continued to play a vital role in offering respite and wellbeing support for staff operating in high-pressure environments.
We also took steps to strengthen physical safety measures across the Trust by reviewing workplace environments for potential hazards, reinforcing compliance with health and safety regulations, and increasing training on conflict resolution and violence prevention to protect staff from harm.
During 2024/25, a significant focus was placed on addressing and reducing sexual harassment in the workplace. As part of this work, we introduced a comprehensive sexual safety policy, launched new e-learning modules on sexual harassment, and ran proactive communication campaigns to raise awareness and drive cultural change.
To monitor progress and identify areas for further improvement, we conducted our annual workplace behaviour survey in February 2025. The results showed:
- A 2% decrease in reported experiences of sexual harassment
- A 20% reduction in reports of bullying and harassment compared to the previous year
- Rates of bullying, harassment, or discrimination related to protected characteristics stabilised between 3–10%.
To support and sustain this progress, we established a sexual safety working group during 2024/25, which leads the rollout of a Trust-wide awareness campaign in 2025. This work supports EEAST’s pledge under the sexual safety charter and will be underpinned by the continued implementation of supportive toolkits, guidance, and targeted communications.
Our focus remains clear: to foster a workplace where every individual feels safe, respected, and empowered to speak up.
Health and Wellbeing
The health and wellbeing of our staff remained a core priority throughout 2024/25, with a continued focus on mental health support, staff engagement, and building resilience across the organisation. A wide range of initiatives were implemented or enhanced to create a safe, supportive, and responsive environment for all colleagues.
Key Developments during 2024/25
Expansion of support networks We increased the number of TRiM practitioners, mental health first aiders, wellbeing champions, and menopause mentors available across the Trust. A refreshed wellbeing champions programme was launched and embedded into local teams, supported by monthly all staff champion check-ins to ensure ongoing peer support and collaboration.
Occupational Health In January 2025, we successfully launched an internal occupational health service, designed to improve efficiency, accessibility, and responsiveness. This marked a significant step toward providing more personalised and timely support for staff.
Policy Development A new managing stress at work policy was approved, with an accompanying individual stress risk assessment template published in March 2025.
Health and Wellbeing Service Group A dedicated service group has been established and meets monthly to coordinate strategic wellbeing efforts and share best practice.
Mental health awareness training Delivered in partnership with MIND, our mental health awareness training exceeded its annual targets and continues to be offered into 2025/26. As of March 2025, we have had 328 attendees.
We procured a new mental health first aid provider with 173 mental health first aiders now operational. Big Dog, Little Dog (BDLD), which received excellent feedback.
A mental health awareness video, produced in collaboration with Magneto and Trust staff, was previewed at the people services away day in March 2024 and officially launched at the welfare wagon event in May 2024.
Digital Innovation We launched the “Time for Me” wellbeing platform and app, powered by Hapstar, on 1st June 2024. This tool offers staff centralised access to health and wellbeing resources, self-help tools, and support networks.
Welfare Wagons Now fully operational and deployed across the region, we have six welfare wagons in place—each equipped with refreshments, fridges, water units, and external power lines. These vehicles offer vital support at hospital handovers and at station locations, providing a safe space for conversation and signposting to wellbeing services. The programme has grown to include 40 trained volunteers, with more being recruited.
Audits and Evaluation An internal audit of our health and wellbeing efforts, conducted by TIAA in May 2024, provided valuable insights to inform ongoing improvements.
Suicide Prevention and Trauma Support We completed a new suicide prevention support guide for managers, along with a standard operating procedure for prevention and postvention support. A full review of our TRiM (trauma risk management) service is underway, with expert support from Professor Jennifer Wild (University of Canberra) and The Ambulance Staff Charity (TASC).
Spiritual and Cultural Support We are exploring the recruitment of a pastoral support officer to lead a team of volunteers from multiple faiths, providing a more inclusive alternative to the traditional chaplaincy model and better meeting the diverse needs of our workforce.
Communication and Engagement We launched a new wellbeing network and accompanying monthly newsletter, helping staff stay informed, connected, and engaged with our wellbeing agenda.
Looking Ahead to 2025/26
As we move into 2025/26, our focus will shift from expansion to quality and sustainability. We aim to:
- Continue promoting the Time For Me platform, driving registration and regular usage through ongoing communications and content updates.
- Maintain momentum in welfare wagon utilisation, expanding our volunteer base and optimising deployment based on staff needs.
- Launch the health and wellbeing passport and directory of support, aligned with the Trust’s Time to Lead initiative, by the end of March 2025.
- Ensure the success and effectiveness of our new in-house occupational health team through ongoing monitoring and collaborative working.
Our work in 2024/25 reflects a strong and sustained commitment to the wellbeing of our people—ensuring they are supported, valued, and empowered to thrive at every stage of their career.
Staff Experience
Providing staff with opportunities to share their experiences, insights and views is an integral part of a positive employee experience. Annual and quarterly staff surveys along with forums of engagement provided by staff networks and our local sector change networks, supported a culture of listening, engaging and supporting our colleagues. It was an essential component of our organisation development plan, which combined multiple initiatives to improve, measure and monitor our cultural improvement.
Annual Staff Survey 2024
The NHS National Staff Survey provided an annual opportunity for staff to share how they feel about their experience of working at EEAST. We conducted fieldwork during October and November 2024 which generated participation of nearly 50% of our workforce.
Our national staff survey results showed that EEAST remained the number one ambulance trust, for the third consecutive year, for the rate of improvement shown across all survey questions. 97% of our responses were either the same or had shown improvement compared to the previous year.
The national staff survey results have been shared widely across the Trust and teams have been working on a ‘Listening into action’ programme designed to engage and co-create action plans following staff survey feedback.
Safety at work
We focused heavily on improving the safety of staff at work. One area of focus was on reducing the sexual harassment of staff, through proactive communication campaigns, introducing a new sexual safety policy and implementing new e-learning modules on sexual harassment.
We conduct an annual workplace behaviour survey to help measure rates of harassment, discrimination and bullying within the Trust. In the latest survey, issued in February 2025, we saw rates of sexual harassment declining 2% from the previous year, bullying and harassment declined 20% from the previous year and our rates of discrimination, bullying or harassment related to a protected characteristic stabilising between 3-10%.
Education and Training
EEAST had 726 staff on an apprenticeship during the last year. 360 completed in the year resulting in a 93% achievement rate, which was a significantly favourable position on the average achievement rate across all industries of 54%, and above the government target of 67%.
Our paramedic degree apprenticeship resulted in 36% achieving a first-class honours degree and a further 53% achieving an upper second-class award classification. Across our apprentice Emergency Medical Technician programmes 38% achieved a distinction, 38% achieved merit and 24% achieved a pass.
We launched a second paramedic degree apprenticeship with the University of Bedfordshire to complement our offer from the University of Cumbria. The Trust secured £5 million in levy donation from outside organisations to support the development of our people.
We also worked with our five local universities to offer 250,000 hours of placement activity to student paramedics on placement with us. We have delivered over 400 emergency driving courses and delivered update training to staff across the region.
£631,000 was invested in CPD development programmes for our staff, with over 380 specialist resuscitation programmes delivered with our Critical Care Air Ambulance charity partners. We upgraded our estates with a brand-new training facility at the Bury St Edmunds hub in Suffolk.
EEAST has been approved as an independent education provider of apprenticeships and is starting delivery of our in-house emergency care assistant and emergency contact handler apprenticeship programmes. With partners we are developing an industry specific clinical leadership degree which will launch in September 2025.
We are developing a new education site to deliver more paramedic degree apprenticeships and have 150 spaces to enhance the skills of experienced emergency care assistants to support them to qualify as emergency medical technicians. There are a further 150 spaces for experienced emergency medical technicians to upskill to become paramedics.
Colleague Experience: Freedom to Speak Up
During August 2025, the Trust transitioned to an external Freedom to Speak Up provider, the Guardian Service.
The Guardian Service has delivered comprehensive support to all EEAST staff 24 hours per day, seven days per week, since August. This service maintained complete confidentiality or anonymity, with guardians accommodating staff consultations through multiple channels: in-person meetings, Microsoft Teams conferences, or telephone calls to address any Freedom to Speak Up concerns.
Over the last three years, EEAST’s FTSU team managed 661 cases. Of the 37 received in Quarter 1 of 2024, 32 have been managed and closed at the point of transfer and the remaining 5 active cases were passed to the Guardian Service with permission from those involved.
During the period of August 2024 to February 2025, Trust personnel raised 144 concerns via the Guardian Service. The primary themes identified among these concerns were system and procedural issues, behavioural and interpersonal challenges, and management-related matters.
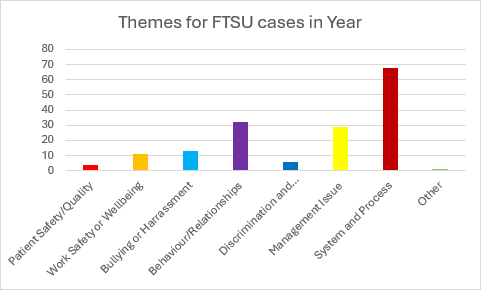
Analysis of reporting preferences indicates that 45.83% of staff who raised concerns through the Guardian Service requested complete anonymity. Additionally, 29.86% authorised escalation with their names disclosed, while 12.50% opted for anonymous escalation of their concerns.
The Trust's two dedicated Guardians will often visit various stations and other locations. They maintain regular consultations with the Board to discuss prevalent themes of concerns, exemplary practices, and strategic recommendations. They report to the Board every other month and quarterly to the Raising Concerns Forum.
Our volunteers
Volunteers and co-response
A variety of volunteering opportunities were available across EEAST. These included community engagement groups, welfare wagon volunteers, research volunteers, military co-responders, community first responders, emergency responders. All our volunteers undertake diverse roles and opportunities within EEAST and provide a valuable service for staff and patients.
Over the past year, we have integrated our volunteers onto a single management platform, so that they all have access to the same resources. This platform has been funded through the East of England Charity, to enable access to all volunteers in turn improving communication flow and ability. This has been a fundamental part of the standardisation volunteering and the development of the volunteer hub. This has enabled standardised safer recruitment and the development of role descriptions for all roles.
Community first responders
Community First Responders are volunteers trained and equipped to provide care to patients in the community. This can be through the lifesaving care of patients or supporting non-injured patients within the community who have fallen and need some assistance in getting up. Over the past year we have trained over 130 new volunteers to respond within the community. Our Community First Responders have provided over 230,000 hours of provision across the regions, attending over 26,110 patients through the year, including over 20 patients who have been successfully discharged from hospital following a cardiac arrest. During the year we have upskilled our volunteers to be able to deliver blood sugar testing for patients in the community. Through a partnership with NHS Charities Together we have been able to upskill our volunteers to provide non injury falls capability with training and lifting equipment, and cars to enable them to respond to communities where there may not be a voluntary response available.
Military co-responders
Our 100 military co-responders delivered care across the region to over 2,077 patients, and provided 4,895 hours from their bases of RAF Marham, Honington, Wyton and Henlow. Over the year, we provided continuing professional development sessions for these volunteers to enable them to respond either, using an ambulance or a rapid response vehicle, to a wide cohort of patients whilst recruiting new responders into the teams.
Fire Service co-response
EEAST continued to develop its collaborative activity across the region with county-based Fire and Rescue services supporting EEAST, at medical calls. Fire crews predominantly attend cardiac arrest calls in rural areas and arrived ahead of EEAST crews at 70% of incidents. EEAST in collaboration with the Fire service will continue to build on the model to improve the response we can provide to our patients across the region.
Emergency responder scheme
Working in partnership with the Beds & Herts Emergency Critical Care Scheme we launched a new volunteering opportunity for people to be part of a new team of volunteers which can respond to patients in a rapid response vehicle under emergency response driving conditions with additional clinical skills greater than that of a Community First Responder. These teams also attended trauma related incidents such as road traffic accidents, unlike a Community First Responder.
This team of 30 volunteers has delivered 1,938 hours and attended 730 patients on behalf of EEAST. We will be expanding our partnership with another critical care charity to expand this provision across the region with the view of proving onward development opportunities across the region for clinical volunteers.
EEAST Heart
Our volunteers provided community education through EEAST Heart and have provided training to over 6,700 people and attended county and local shows, fetes and events to promote the ambulance service, volunteering and training in basic life support, and raising funds for our charity to provide more equipment and support for the provision across the region.
Patient safety
Since launching the patient safety incident response framework (PSIRF) in September 2023, the patient safety team has reviewed a total of 98 patient safety events, not inclusive of system delay incidents of which there were a further 55 delay incidents meeting the moderate, severe or fatal level of harm. System delays continued to be reviewed through the urgent and emergency care forums with the Integrated Care Boards within each sector across the region.
In the past year, the patient safety team completed two thematic reviews (PSII’s)
- Missed ST elevation myocardial infarctions
- Non conveyance incidents.
The team has embraced the PSIRF methodology by engaging with patient, staff and relatives that have been involved in, or affected by incidents.
All reports completed have been shared within EEAST, with patients and families, external stakeholders and the national ambulance risk and safety forum (NARSF). The feedback on the work EEAST produced has been positive. The non-conveyance report resulted in enquiries from other services relating to the ‘safe discharge care bundle’ and they intend to implement similar processes in their organisation.
This report included a patient story from a discovery interview and was praised by the quality governance committee for the way the data was presented, and how patients had been part of the development of the recommendations.
Following our the initial PSIRF plan for the past year, we are implementing a review of the reporting data from the past 12 months to support the preparation of the PSIRF plan for the financial year 2025/26, which was approved at the executive clinical group in January 2025. The four PSII themes in the plan are:
- Medication errors – IM adrenaline 1:1000
- Discharge of abdominal pain in the prehospital setting
- Resuscitation decisions – decisions not to start resus and decisions to stop once resus has commenced
- Patient injury whilst in the care of EEAST, due for completion in April 2025
PSII reports are complex, including data from many reported incidents and including views and information from staff, patients and relatives. The aim for 2025/26 is to complete one PSII per quarter. If during the year issues or challenges are identified through incident reporting trends the plan may change, the PSIRF plan is a fluid document which can be amended with additional themes if necessary. The important element at the centre of this is to learn and improve the standards of care, safety and experience of patients.
Reporting
Reporting from patient safety events was completed on a monthly or every other month basis, submitted via the quality report and to the patient safety and experience group, the compliance and risk group and the quality governance committee. Patient safety data was also shared nationally via NARSF monthly.
Incident Review Panel
The panel met at least once, and up to three times per week, to discuss incidents and assess the level of harm EEAST may have contributed towards an incident, to identify the patient safety or health and safety harm incidents and complaints that are key to organisational learning.
Harm was assessed using the learning from patient safety events guidance set out by NHSE. The panel comprised of a multidisciplinary group of senior clinical colleagues and was attended by subject matter experts who provided a balanced and independent view of specific clinical matters, as required.
Action Setting Group
The action setting group met twice per month, to review reports and recommendations from safety reviews and ensure that SMART actions were set to drive organisational improvement and avoid recurrence of incidents in the future. This group also monitored the previously set actions to ensure timely manner completion.
Learning from deaths
Learning from deaths workload was completed by clinical staff on alternate working duties, supported by the head of patient safety, as EEAST was mandated to complete 40 structured judgement reviews per quarter. Compliance on this figure was exceeded in each quarter of 2024/25, and to date. The completion of structured judgement reviews allowed for the identification of emerging themes and trends which may require further review as well as highlighting areas of excellence.
System delay process trial
In quarter three of 2024, the head of patient safety worked jointly working with patient safety colleagues at the Suffolk and North East Essex Integrated Care Board to trial a new system delay review process. The success of this has led to the intention to expand this across the region throughout 2025 and allows all members of the health economy to review incidents reflective of the PSIRF approach and allows for wider learning.
Sharing learning
Learning was shared across EEAST through a monthly newsletter “Safety Matters”, a popular publication shared via the communications team to all staff in the Trust. In the coming year there are plans to utilise the JRCALS+ app to provide clinical updates. Additionally patient safety updates are sent to staff by email or placed on the intranet. Safety Matters videos and podcasts are also available on Trust’s You Tube channel.
Engagement
The patient safety team held engagement events across the region during 2024/25, delivering patient safety training to existing staff and new recruits to the organisation and newly appointed managers.
Patient safety partners
EEAST had two patient safety partners that attended a variety of meetings as representatives of the community, who also met with safety and experience teams and ICB colleagues. This role was mandated for organisations under the PSIRF guidance.
Reporting system
EEAST used the Datix system to report incidents and during October 2024, moved to Datix DCIQ, access to previous reports on the previous datix system remained accessible for reporting purposes. This version of the product provides greater opportunities to use the information recorded to identify key themes and trends. The system also records complaints and legal claims and inquests allowing the links to be made across these connected elements of our work.
Non-Emergency Patient Transport Services
Last year, EEAST provided non-emergency patient transport services (NEPTS) across Hertfordshire, West Essex, Bedfordshire, Luton and North East Essex.
Our non-emergency patient transport team consists of highly trained healthcare professionals, drivers, and support staff who are committed to delivering exceptional care. They provided accessible and comfortable transportation for patients who were unable to travel to medical appointments independently.
We understand that the journey to and from medical appointments can be stressful, especially for those with mobility challenges or health concerns. That's why we've tailored our services to prioritise the patient's comfort and safety. Our vehicles are equipped with medical equipment and staffed by caring professionals who ensure patients receive the care they deserve during their journey.
Delivery
Our patient transport service has over 350 team members across our three contracts, with a fleet of over 130 vehicles. During 2024/25 our patient transport service delivered over 401,188 journeys, including escorts.
CallEEAST, our contact centre, managed all patient screening and bookings by telephone and online. During 2024/25 we received 333,878 telephone bookings and 21,502 online bookings. One focus for the year ahead will be to look at using our online systems to increase the volume of online bookings which will further improve bookings. Our control rooms situated in Bedford, Stevenage and Chelmsford managed the coordination and dispatch to patients and queries those patients had via the phone.
As well as our pre-planned and ‘on the day’ journeys for patients of various mobility types who attended medical appointments, the patient transport service played a crucial role in supporting the wider system flow with transfers and discharges from hospital. Last year, 15% of our total journeys were discharges, this was an increase from the previous year, where 13.5% of all journeys were discharges.
Performance
Last year, EEAST introduced an improved management structure for the patient transport service, with the appointment of a dedicated contract manager for each contract, including oversight from the contracts lead. This investment brought contractual and financial stability and enhanced working relationships between EEAST and our commissioners. Each contract was monitored through monthly contract review meetings to measure performance against agreed key performance indicators (KPIs) and shared innovative approaches to improve our service and patient experience.
2024/25 was a year of transformation for our patient transport service. We collaborated with Integrated Care Board partners to design a sustainable, system focused service which prioritised patient needs over commercial targets and supported regional improvements in health care. This work was managed over several programme boards and significant progress has been achieved with EEAST looking forward to the introduction of these new contracts over 2025/26. The design of each service contract is unique, based on journeys undertaken by each mobility type, over time. EEAST developed a new patient transport service modelling application that allows for statistical modelling of activity to estimate workforce and vehicle requirements.
Mapping tables were used to map vehicle mobility types to variables such as number of staff per vehicle, average speed travelled and loading and unloading times. These variables were combined with the average mileage estimates to calculate average journey times. This model has been crucial in the co-design work to allow us to conduct scenario planning and to determine the parameters within which the contracts should operate to be effective.
EEAST is looking forward to continuing this innovative and collaborative approach to patient transport services in the year ahead to continue to strive to improve efficiencies and deliver high quality care for all our patients.
Urgent and Emergency Services
EEAST's performance was challenged over the 2024/25 financial year, prompting the development of the Organisational Performance Improvement Plan (OPIP) to drive measurable improvement.
The OPIP set out a clear framework underpinned by a series of key assumptions across demand, capacity, and efficiency. In terms of demand, the plan anticipated a 3.10% growth in face-to-face responses over two years. For capacity, the assumptions included timely delivery of the clinical workforce plan, a 12-week period for staff to become work-effective, and controls on weekly abstractions, turnover (not exceeding 10.5%), and operational overtime (averaging 4,300 hours/week).
The plan also relied on consistent private ambulance support, providing an average of 5,051 hours/week. Under efficiency, EEAST aimed to limit hospital handover delays to 3,000 lost hours per week, maintain Job Cycle Time (JCT) below 2 hours and 19 minutes, and closely monitor Vehicle Off Road (VOR) metrics. These assumptions formed the foundation for tracking and enhancing operational performance through OPIP.
Response Times:
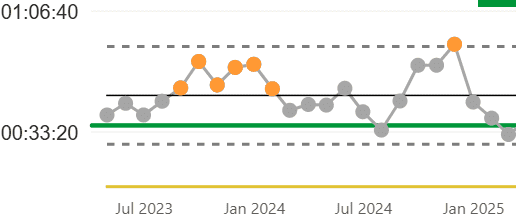
The table displays mean response times for different emergency categories over a 12-month period (March 2024 – March 2025). The total column summarises the overall average response time for each category. Key Observations:
- Category C1 (Most Urgent Cases) maintained a consistent response time, averaging around 9 minutes across all months, with a total of 00:09:08.
- Category C2 (Urgent but Less Critical Cases) showed fluctuations, peaking at 00:57:20 in December 2024 but averaging 00:42:39 overall.
- Category C3 (Less Urgent Cases) had response times ranging from 01:39:49 to over 3 hours, with an overall mean of 02:20:43.
- Category C4 (Non-Urgent Cases) consistently had the longest response times, exceeding 3 hours in multiple months, with an overall mean of 03:32:21
March 2025 saw the best response times for the year in all categories.
- C1: 00:08:32
- C2: 00:32:47
- C3: 01:38:57
- C4: 02:30:00
The worst response times were recorded in December 2024; this was expected due to seasonal pressures including increased demand.
| Mar24 | April 24 | May 24 | June 24 | July 24 | Aug 24 | Sept24 | Oct 24 | Nov 24 | Dec 24 | Jan 25 | Feb 25 | Mar 25 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C1 | 00:08:49 | 00:08:57 | 00:09:04 | 00:09:19 | 00:09:01 | 00:08:40 | 00:09:22 | 00:09:42 | 00:09:39 | 00:09:47 | 00:08:53 | 00:08:45 | 00:08:32 | 00:09:08 |
| C2 | 00:39:06 | 00:40:43 | 00:40:32 | 00:45:11 | 00:38:42 | 00:33:38 | 00:41:41 | 00:51:32 | 00:51:33 | 00:57:20 | 00:41:23 | 00:36:55 | 00:32:47 | 00:42:39 |
| C3 | 01:57:19 | 02:05:57 | 02:21:08 | 02:30:49 | 02:05:17 | 01:45:51 | 02:22:05 | 03:03:39 | 03:04:59 | 03:30:03 | 02:05:12 | 02:02:55 | 01:38:57 | 02:20:34 |
| C4 | 02:42:18 | 03:07:56 | 03:22:05 | 03:51:50 | 02:52:40 | 02:42:56 | 02:55:28 | 04:24:56 | 04:30:20 | 05:11:51 | 03:22:51 | 03:29:18 | 02:30:00 | 03:32:21 |
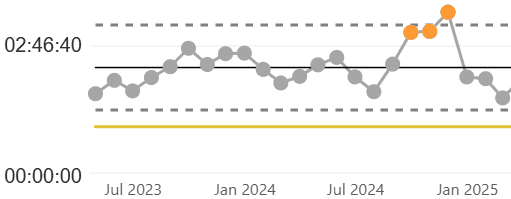
C1 Response Times
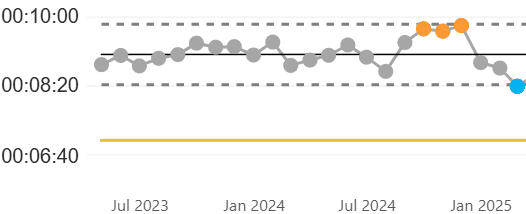
C2 Response Times
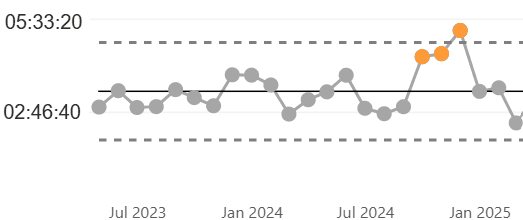
C3 Response Times
C4 Response Times
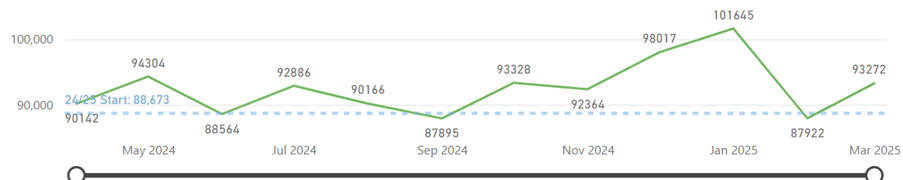
Operational Resourcing
Key Observations
- The weekly patient-facing staff hours have fluctuated throughout the year.
- The target for 24/25 was set at 88,673 hours, which was exceeded in multiple months.
- The highest recorded PFSH was 101,645 hours in January 2025, indicating peak workforce availability. This is planned throughout the winter months.
- The lowest was 87,895 hours in September 2024, slightly below the target.
Workforce availability is improving. The total patient-facing staff hours has increased in March 2025 compared to February, suggesting efforts to increase staffing levels are working.
Bedfordshire and Luton have significantly lower staffing hours compared to other regions, which is in line with the lower population (therefore, demand) in the sector.
Fluctuations exist but 9 out of the 12 months for 24/25 remained above target: While some months (e.g., September 2024) dipped below target, overall staffing levels have remained strong, particularly in early 2025.
Over the past year, EEAST has implemented several initiatives to enhance staffing levels and workforce effectiveness:
Recruitment and Retention Efforts: EEAST has successfully reduced staff turnover through a well-planned strategy, maintaining a strong workforce with valuable experience and skills, while saving on recruitment and external staffing costs.
Implementation of the 'Time for Me' Wellbeing Platform: In May 2024, EEAST launched 'Time for Me,' a platform powered by Hapstar, to support mental health and wellbeing. With nearly 700 employees and volunteers registered, over 60,000 wellbeing data points have been captured, enabling targeted support and early intervention.
Adoption of the NHS Long Term Workforce Plan: EEAST aligns with the NHS Long Term Workforce Plan, focusing on expanding education, training, and recruitment to ensure a sustainable and resilient workforce.
Implementation of E-Rostering and Effective Job Planning: EEAST uses electronic rostering and effective job planning to ensure appropriate staffing levels, enhancing productivity and patient care.
Call Pick Up
Key Observations:
Mean Call Pick-Up Time)
- Best performance: February 2025 (00:00:04) – indicating fast response times.
- Worst performance: December 2024 (00:00:11) – slower response times.
- Target: 00:00:10, meaning most months are within or near target.
95th Percentile Call Pick-Up Time
- The slowest response was recorded in December 2024 (00:01:03).
- The fastest response was February 2025 (00:00:33).
- The target is 00:00:40, meaning some months exceed this.
Percentage of Calls Exceeding 2 Minutes
- Best month: February 2025 (0.61%), indicating excellent performance.
- Worst month: February 2024 (2.35%), where more calls took over 2 minutes to be answered.
- Target: 6%, meaning all months are performing well within acceptable limits.
Trends and Insights:
- Overall Improvement: Call pick-up times have improved over time, with recent months showing faster response times.
- December 2024 Struggles: This month had the slowest call pick-up times, due to seasonal demand increases.
- Performance Close to Targets: Most months meet or are very close to target metrics, indicating effective operational management.
EEAST has undertaken several initiatives to enhance call pick-up times and overall responsiveness.
Workforce expansion: In the past year, EEAST has significantly increased its staffing levels, recruiting 717 new personnel, including 139 call handlers. This strategic expansion has led to notable improvements in call response metrics.
Technological advancements: EEAST has implemented the Mobile Data and Vehicle Solution (MDVS) program, a national initiative replacing outdated on-ambulance technology. This system enhances communication and data access for frontline staff, supporting quicker and more informed decision-making during emergencies.
Retention and wellbeing initiatives: Recognising the importance of staff retention, EEAST has focused on fostering a supportive work environment and promoting a culture of well-being. These efforts have led to a decrease in call handler turnover, with average weekly departures dropping from four to just under two. Please see further detail on recruitment & retention in the ‘Our People’ section of this report.
These combined efforts reflect EEAST's commitment to improving emergency response times and enhancing patient care through strategic recruitment, technological innovation, and staff support.
Hear and Treat
Key Observations:
Monthly Trend
- The hear and treat percentage has shown a gradual increase over time, starting at 8.70% in May 2024 and rising to 13.15% in March 2025.
- The target for 23/24 was 13%, which has been met in the latest data (March 2025).
Sector performance
- Bedfordshire and Luton had the highest hear and treat % in February 2025 at 15.74%.
- Norfolk and Waveney followed closely at 14.03%.
- The total hear and treat % across all ICBs for February 2025 was 13.15%, showing improvement.
- Suffolk and North East Essex had the lowest hear and treat % at 11.30%.
Conclusion
Our hear and treat % is steadily increasing, showing effective intervention strategies. Some ICBs outperform others, suggesting opportunities to support lower-performing regions.
The 24/25 targets are being met, which is a positive indicator of operational efficiency.
Over the past 12 months, EEAST has implemented several initiatives to enhance its Hear & Treat services, aiming to provide timely and appropriate care while optimising resource utilisation:
Introduction of the Unscheduled Care Coordination Hub (UCCH):
In September 2023, EEAST, in collaboration with NHS Norfolk and Waveney Integrated Care Board (ICB) and Integrated Care 24, launched the UCCH. This initiative focuses on reviewing 999 calls to coordinate alternatives to ambulance dispatches, enabling patients to receive appropriate care at home and freeing up ambulance capacity for other emergencies.
Since its inception, the UCCH has successfully diverted calls from the ambulance service, improving patient outcomes and system efficiency. The UCCH's efforts were recognised with the 'Best Contribution to the Improvement of Urgent and Emergency Care' award at the HSJ Partnership Awards 2025.
Implementation of the Single Point of Access (SPA) Scheme:
Building upon the UCCH framework, EEAST introduced the SPA scheme, allowing clinicians to make a single phone call to:
- Consult with a clinician to determine the most appropriate care pathway for a patient.
- Review and adjust patient medications through discussions with senior clinicians.
- Enrol patients into 'virtual ward' care, providing hospital-equivalent treatment at home.
Organisational Performance Improvement Plan (OPIP)
EEAST has prioritised increasing Hear & Treat rates as a key component of its OPIP. This focus is designed to improve response times for Category 1 and Category 2 patients by efficiently managing demand through enhanced telephone triage and clinical assessment services. The OPIP also emphasises reducing job cycle times and utilising community care pathways to avoid unnecessary hospital admissions.
Job Cycle Time
Job cycle time (JCT) represents the total time taken to assist a single patient. The shorter the time taken the more patients can potentially be assisted. The largest part of the JCT is typically the on-scene times and these are within our control. Reducing on-scene times is crucial for providing care that aligns with the standards of other UK ambulance services and ultimately benefits the patient.
Completed actions include:
- Roll out of Organisational Information portal (OIP), This action allows the visibility of individual performance and is planned for rollout alongside a framework of performance appraisals. OIP has now been rolled out Trust wide and is monitored locally by the management teams and progress reviewed through the regular OPIP meetings.
- Delivery of bespoke training on 'quality efficiencies on scene’ to all operational areas. This action ensures that staff are briefed on the positive patient benefits to shortened on scene times.
- Education programme on clinical best practice on scene decision making. Led by the clinical leads, this education programme is designed to support staff outside of the normal on scene time ranges. All sectors have produced plans to roll out education.
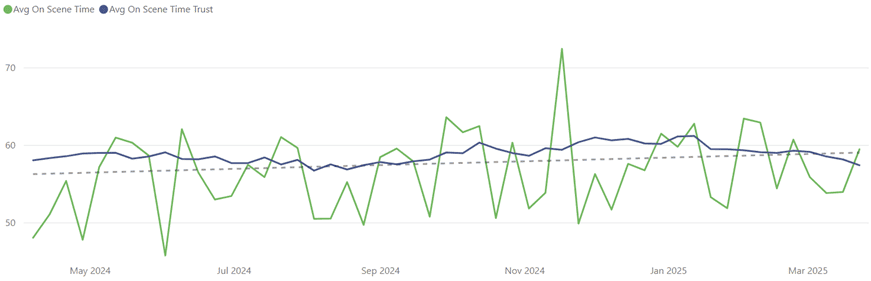
The below graph tracks average On Scene Time (OST) in minutes, which represents the duration emergency response vehicles spend at the scene of an incident before leaving.
- The average OST shows fluctuations, with an increasing trend observed towards late 2024 and early 2025.
- Saturday and Sunday have the highest OST, suggesting weekend pressures impact response efficiency. This is due to increased demand and reduced admission avoidance options.
- Wednesday has the lowest OST, which due to resource allocation driven by rota design (rest days after covering weekend shifts). It is also common that alternative care pathways are more accessible on Wednesdays, the increased demand on Mondays and Tuesdays, caused by limited weekend service provision, eases by midweek, allowing for quicker referrals and reduced OST.
EEAST has implemented several initiatives aimed at reducing on-scene times and enhancing patient care.
EEAST has introduced two innovative stroke care schemes:
Video Triage Ambulance clinicians can connect via FaceTime with senior stroke consultants while on scene, enabling rapid decision-making. This approach has reduced the time from hospital arrival to scanning from 22 minutes to 2 minutes, and from arrival to treatment from 66 minutes to as little as 9 minutes in the fastest cases.
Mobile Stroke Unit This specialised ambulance is equipped with advanced diagnostic tools, including a CT scanner, allowing for immediate blood analysis and stroke diagnosis on-site. Early identification facilitates faster treatment decisions and reduces delays associated with hospital transfers.
Incident Messaging Technology EEAST has implemented the Mobile Data and Vehicle Solution (MDVS) program, a national initiative replacing outdated on-ambulance technology. This system enhances communication and data access for frontline staff, supporting quicker and more informed decision-making during emergencies.
Enhanced Connectivity EEAST is piloting the Hybrid Connex system, which combines 4G, 5G, and satellite connections to ensure continuous communication for ambulance crews, even in areas with poor cellular coverage. Reliable connectivity enables faster access to patient information, supports real-time consultations with specialists, and improves navigation to incident locations, all contributing to reducing on-scene times.
These initiatives reflect EEAST's commitment to leveraging technology and strategic partnerships to improve response efficiency and patient outcomes.
Sickness levels have fluctuated over the past 12 months, with expected peaks observed in August and December 2024. These peaks are linked to school holiday periods and a rise in seasonal illnesses. The most common causes of absence across EEAST have been mental health-related conditions, musculoskeletal issues, and chest and respiratory illnesses.
The most noticeable peak was 11.20% in December 2024. The highest sickness rates are observed in Norfolk & Waveney (up to 12.43%) and Mid & South Essex (up to 12.40%), with the lowest recorded in Bedford and Luton (5.31%).
To improve sickness absence rates, several measures have been implemented including reviewing shift patterns, improved wellbeing and managerial support and enhanced flu and COVID-19 vaccination programs to reduce seasonal illnesses.
Out of Service
Key Objectives:
Reduce weekly total out of service (OOS) hours – Measure total out of service time as a percentage of vehicle hours for DSA & RRV vehicle types. Improve (reduce) cohorting out of service hours – focuses on the time lost due to cohorting.
Performance Summary
- The overall average OOS percentage for the year 25/26 is 7.88%.
- Out of the 7.88%, the average cohorting OOS percentage (4.9) is 1.02%.
- The highest OOS percentage was 9.14% in January 2025, while the lowest was 7.12% in July 2024.
- Cohorting OOS percentage peaked at 1.68% in December 2024 and remained below 1.5% for most months. However, EEAST’s target is 0% for cohorting but due to increased arrival to handover times, it has become a necessity at certain acute hospitals.
- The OOS percentage has shown an increasing trend towards early 2025. This is correlated to an increase in cohorting and recovery from the festive period. Cambridgeshire and Peterborough and Norfolk and Waveney are particularly high-risk areas, with OOS rates nearing 12%. These are also the two areas with the highest cohorting numbers.
EEAST has implemented several strategies to reduce ambulance out-of-service times, ensuring quicker responses to emergencies.
Implementation of the "Handover 45" Policy
Collaboration with Hospital Partners EEAST works closely with hospitals to streamline patient admissions and reduce handover delays. By enhancing communication and coordination, they aim to minimise the time ambulances spend waiting to transfer patients, thereby increasing availability for other emergencies.
Deployment of Alternative Response Vehicles To ensure that resources are used effectively, EEAST utilises various types of response vehicles, including rapid response cars and community first responder units. These vehicles can often reach patients more quickly and handle certain emergencies without the need for ambulance transport, thereby keeping ambulances available for more critical cases.
Implementation of Automatic Stand-Downs for Meal Breaks EEAST has introduced an automatic stand-down process for meal breaks, ensuring that crews are marked as out of service (OOS) within five minutes of arriving at the station for their designated break. This system guarantees that all staff receive the appropriate downtime, supporting their well-being while maintaining operational efficiency. By standardising meal breaks, EEAST enhances workforce resilience and ensures a balanced approach to staff welfare and service delivery.
Hospital Handover
Key Objectives:
Reduce Arrival to Handover (A2H) Delays – Measure time from ambulance arrival at the hospital to patient handover. Reduce Handover to Clear (H2C) Delays – Measure time from patient handover to when the ambulance is ready for the next call.
Performance Summary
- Target for A2H is 15 minutes our average is 38:04 minutes
- Target for H2C is 15 minutes our average is 15:00 minutes.
- Worst A2H Performance was January 2025 at 50:01 minutes
- Worst H2C Performance was November 2024 at 16:43 minutes
- Arrival to Handover (A2H) delays are significantly above the target, with no month meeting the goal. This metric is out of EEAST’s control and replies on support from the acute hospitals to improve.
- Handover to Clear (H2C) improved in early 2025, gradually aligning with the target. Geofencing/auto-clear functionality were implemented in December 2024 to enhance Handover to Clear (H2C) times. Since its introduction, a notable improvement has been observed, the automation of the ambulance "clear" status has streamlined the H2C, reducing delays and ensuring a quicker return to service.
EEAST has implemented several strategies to address and reduce patient handover delays at hospitals.
Implementation of Ambulance Handover Units In collaboration with local hospitals, EEAST has introduced Ambulance Handover Units to facilitate quicker patient transfers. For instance, at Southend Hospital, a 12-patient capacity unit was established to expedite handovers, allowing ambulance crews to return to service more promptly. This initiative aims to enhance patient care by ensuring timely medical attention and reducing ambulance turnaround times.
Automatic Handover Protocols EEAST has been working on implementing protocols to automatically hand over patients after a specified period, such as 45 minutes (Handover 45), to enable ambulance crews to respond to other emergencies. This approach is designed to balance the need for timely patient care in hospitals with the necessity of maintaining ambulance availability in the community.
"Handover 45" refers to a policy implemented by EEAST and other ambulance services to address delays in transferring patients from ambulances to hospital emergency departments (EDs). Under this policy, if a patient handover is not completed within 45 minutes, ambulance crews may leave the patient in a designated area within the ED, provided the patient is clinically stable.
Collaboration with Healthcare Partners EEAST collaborates with regulators, commissioners, and hospitals to reduce handover delays. By implementing handover escalation protocols, the organisations work together to identify and address offloading issues promptly, aiming to accelerate care and minimise delays.
Alternative Care Pathways To reduce unnecessary hospital admissions and alleviate pressure on emergency departments, EEAST has developed alternative care pathways. These initiatives include the Clinical Assessment Service, which manages a significant proportion of 999 calls through 'hear and treat' methods, providing advice, guidance, or signposting to other services without dispatching an ambulance. Additionally, partnerships with unscheduled care services and the establishment of a single point of contact for referrals to various community services have been implemented.
These efforts reflect EEAST's commitment to improving patient outcomes and ensuring that ambulance resources are utilised effectively to meet the needs of the community.
NHS England has recognised the importance of reducing hospital handover delays, as they can delay assessment and treatment for patients and compromise safety by reducing ambulance availability for emergencies.
Resilience and specialist operations
Our resilience and specialist operation team was involved in both responding to, and helping EEAST to prepare if, any untoward, adverse or serious major incidents, or terrorist attacks were to happen. The team engaged during the year with 672 local resilience forum meetings and attended 562 safety advisory group meetings.
Although the total number of meetings had decreased slightly, compared to 2023/24, the length of time these meetings are taking had increased. This was especially the case for the safety advisory groups which are now reviewing multiple events during one meeting, rather than having a different meeting for each event, as had been the case, in some areas, in previous years.
Manchester Arena Inquiry
During 2024/25 the department had a dedicated resilience manager reviewing and implementing the learning which came from both the Manchester Arena Inquiry and the Grenfell Tower Fire Inquiry. However, this post’s funding expired on 31 March 2025 and the learning would be embedded into business as usual rather than having a dedicated person looking at it.
EEAST looked at 104 of the 149 Manchester Arena Inquiry recommendations and reported nationally to the association of ambulance chief executives on 77 of them. We worked through the recommendations linking these to the NHS EPRR Core Standards, where appropriate identified gaps in operational practice which we are now working to understand how these gaps can be best filled.
To date the Trust has completed the learning associated with 46 of the recommendations, have 36 in progress and are awaiting a national steer on 22 of the recommendations.
Hazardous Area Response Teams
Hazardous area response teams (HART) respond to patients requiring medical care in any hazardous environment. The team also support ambulance crews responding to patients who are not necessarily in a hazardous area but who are hard-to-reach or where multiple clinicians are required. Over the year, the two teams within the East of England have responded to patients taken unwell or injured in and around water, at height and within confined spaces; not to mention those who have become injured in the middle of muddy fields!
During the 2024/25 financial year, the East of England HART assets responded to 3620 separate incidents across the region. This included HART colleagues supporting partner agencies at protests as well as supporting the police with medical mitigation where numerous hazardous substances were found in private dwellings.
Specialist Operations Response Team
In addition to the two HART capabilities on duty 24/7, the Trust was required for there to be at least 35 Specialist Operations Response Team (SORT) staff on duty between the hours of 06:00 and 02:00 of each day. During 2024/25 the Trust achieved this 95.2% of the time.
SORT staff are staff who are employed within the Trust, normally on front line duties, but who would volunteer to respond to a major incident to support the Trust with its capabilities of responding to a marauding terrorist attack or following the release of a chemical, biological, radiological or nuclear (CBRN) material. As well as requiring there to be 35 SORT staff on duty the Trust is also required to have 290 staff trained at any one time in the SORT key elements.
EEAST maintained the number of SORT trained staff, however, to allow this to occur the Trust had to self-fund a small number of additional staff’s training, thus allowing a small buffer for staff who leave the team at short notice or who are off work and not able to complete their regular revalidation training.
Exercises
We ran multiagency exercises bringing partners from police, fire, health and other agencies together with us to respond to a potential marauding terrorist attack occurring. For these exercises, we used a disused hospital as a “fictitious town”. During the 20 exercises, which predominantly ran during September and October 2024, just over 1,700 emergency service responders improved their clinical and command skills and gained a better understanding of how an incident of this nature would be managed and care delivered to those in need.
The exercise has generated over 80 learning points, those relating to the Ambulance Service will be reviewed and implemented into business as usual. One of the learning points was to build a tabletop exercise for the wider health economy looking at the catastrophic impact an incident of this nature would have. This has now been completed and is helping build the resilience of the wider health responders, rather than just the Ambulance Service.
While we hope these skills are never needed within the East of England, recent high profile media coverage has shown us that people, living within the region, have planned to carry out such attacks, which if had been seen through, would have had catastrophic consequences.
Core Standards
Each year English NHS trusts complete a statutory annual self-assessment and review compliance against the NHS Emergency Preparedness, Resilience and Response Framework, in line with the Civil Contingencies Act 2004.
We maintained our overall compliance as substantial and compliance with interoperable capabilities was also rated as substantial.
However, the Trust did record that it was non-compliant against the requirements to have sufficient resources to allow the Trust to plan, prepare and respond to a Major Incident. This was on the back of the learning from the Manchester Arena Inquiry where the Trust has requested additional funding, but unfortunately not yet received any.
To ensure continual development and following external audit, the department maintains and manages an action plan to ensure the Trust develops and can deliver a high-level service.
Digital Development
Investment and improvement of our digital infrastructure
A key achievement last year was the successful upgrade of EEAST’s digital internet-based telephony platform. Not only did this provide a reliable communications medium for patients, but the system also underpinned the Trust’s hybrid working model where EEAST clinicians were able to operate from any location. As part of the NHS Ambulance Radio Programme, EEAST completed successful migration to the new national mobile data vehicle system (MDVS) which meant installing new communications equipment in over 650 emergency vehicles. The Trust also migrated to a new control room system (CRS) and implemented touch screen technology at all three emergency operational centre (EOC) rooms.
Digital innovation
The Trust introduced robotic process automation last year within the emergency operational centres to direct patients that had a specific condition directly to the most appropriate care pathway. “Marvin” our virtual assistant runs 24 hours a day, seven days a week and has supported over 20 patients per month to receive alternative appropriate care rather than an ambulance being dispatched.
The Trust is planning to achieve a minimum 25% increase in robotic process automation activity in the coming year with expansion to non-clinical areas.
Supporting our people and patients
During 2024-25 EEAST invested in Apple iPad technology with software that digitally records treatment when attending patients and made that information available to receiving hospitals. Three years into that programme EEAST successfully refreshed 5,000 Apple iPads with replacement new devices over a four-month period. In addition, our front-line staff now have access to over 20 clinical applications and resources, such as the national patient record locator, in real time enabling decision making and improving patient outcomes.
Cyber security
EEAST continued to invest in robust protection, identification and recovery countermeasures as the external cyber threat continued to evolve. The Trust produced over two and a quarter million emails and sent an average of three hundred and sixty thousand emails every month. To support this both inbound and outbound active monitoring was established. The Association of Ambulance Chief Executives commissioned an external assessment of ambulance trusts cyber security capabilities late 2024, EEAST was above the national average. The areas for improvement recommendations have been included in the Trust’s planning for the coming year.
Data innovation
EEAST successfully introduced the NHS national ambulance data set into the Trust’s electronic patient record. The data collected supported all stakeholders by providing several benchmarking opportunities to improve efficacy of patient care. The data will identify best practice to drive organisational and clinical improvement as well as gaps in service provision to support better commissioning of services to support patients’ onward care with the most appropriate care provider.
Commercial partnerships
Over the past year, EEAST’s commercial services made significant progress in aligning business units under a unified commercial strategy, focusing on revenue generation, service diversification, and the delivery of measurable social value.
Commercial growth continued to accelerate, and financial contributions exceeded initial forecasts, this growth was underpinned by increased market presence through websites and social media, operational improvements, and strengthened governance frameworks. Through ensuring commercial sustainability, surplus revenue was reinvested by EEAST to enhance patient care and community health outcomes.
CallEEAST
CallEEAST maintained strong operational performance over the past year, it consistently met contractual key performance indicators (KPIs) and achieved a 53% revenue increase year-on-year. The service successfully expanded its portfolio, secured new partnerships with Mid and South Essex Integrated Care Board (MSE ICB), GP surgeries, and private sector organisations.
CallEEAST launched the innovative virtual ward out-of-hours monitoring service in collaboration with Suffolk and North East Essex ICB, West Suffolk NHS Foundation Trust, and East Suffolk and North Essex NHS Foundation Trust. This service from implementation to now has seen significant success in providing support to patients out of hours, and both CallEEAST and virtual ward teams communicated effectively to ensure the continued care of patients admitted to the virtual ward, ensuring vital 24/7 support. CallEEAST will continue into 2025-26 with this provision working closely with partners to continue to improve the service.
CallEEAST has had further success collaborating with organisations such as Ergéa, a leading provider of managed equipment services for the NHS and private healthcare sector. Collectively re-designing the out of hours support service enabling health care professionals across the country to access vital equipment support around the clock. We are continuing the collaborative approach to enhance service offering and user experience.
In early 2025, CallEEAST partnered with multiple new GP surgeries across the United Kingdom, to help implement the change to primary care access online, including with a large GP surgery in London to support this transition and to offset the ‘8am queue’ as experienced across the country.
Looking ahead, CallEEAST will continue to scale its operations and explore new revenue streams, continue to collaborate and design services that yield increased patient experience, efficiency and customer experience.
TrainEEAST
TrainEEAST underwent a strategic transformation, improved financial sustainability and market competitiveness. The service strengthened its commercial offering by:
- Implementing a new leadership structure and embedding a clear commercial vision.
- Diversifying its training portfolio, moving towards specialist trauma and paramedic training.
- Expanding corporate partnerships, securing contracts with Hertfordshire Partnership University NHS Foundation Trust, additional NHS Trusts and emergency service colleagues.
- TrainEEAST has grown its team and invested in trainers to optimise the training experience and course offering.
Future initiatives include:
- Access to work programme – supporting neurodiverse learners through in-house coaching.
- Resuscitation Council UK centre status and the provision of RCUK courses across the region.
- Military conversion pathway – enabling ex-military personnel to transition into emergency medical technician (EMT) roles.
These developments position TrainEEAST as a key contributor to EEAST’s commercial portfolio while delivering essential workforce training to healthcare providers and commercial organisations.
NPAG
NPAG has expanded its footprint, increasing NHS membership and training offerings. Key achievements include:
- Delivering four conferences: Waste, Energy and Sustainability Conference, Theatres and Decontamination Conference, Clinical engineering Conference and National District Nursing Conference
- Development of a Customer Relationship Management (CRM) system to enhance operational efficiency.
- Growth in facilitated workshops and training, ensuring best practice sharing across NHS organisations.
Through its NPAG networks, EEAST achieved award recognition for its waste management strategy, highlighting the significant value and impact of NPAG collaborations.
With over 700 members across 18 specialist groups, NPAG continues to play a pivotal role in shaping healthcare innovation and efficiency across the UK.
Outlook
As we move into 2025-26, EEAST’s commercial services will focus on:
- Expanding commercial partnerships across health and private sectors.
- Driving innovation in contact centre services, digital transformation, and training solutions.
- Maximising social value impact, reinforcing EEAST’s role in supporting wider NHS objectives and community resilience.
- Maximising re-investable surplus back into EEAST.
Sustainability
We made progress last year to embed environmental sustainability across the Trust and to use our influence with our partners and suppliers. Colleagues are increasingly interested in sustainability and working in a more sustainable way.
Our green champions network has 43 active members and continued to grow monthly. Within the network, quarterly meetings were held to give updates on sustainability within the Trust and green champions had the opportunity to present on an initiative they were undertaking. The network had a dedicated MS Teams channel which had weekly posts and channels for discussion. Green champions received a monthly newsletter with training opportunities, webinars, and updates.
Communications and Engagement
Since April 2024, 28 articles have been published on our intranet (East24) which have received a total of just over 8,700 views. Since January 2025, we have published a monthly sustainability and estates newsletter to raise awareness of estates projects, cost saving initiatives and promote sustainability events. Members of the sustainability team presented at the 27 June 2024 and 31 October 2024 Executive Q&A. This provided an opportunity to reach a wider audience, with positive feedback received on both occasions.
Travel questions were added to the quarterly pulse survey in August 2024, with 1,184 respondents. As expected, most staff commute by car (86.5%), but 20.9% of these journeys are under 5 miles providing opportunities to swap these journeys with active or sustainable travel. Travel questions were also included in the national staff survey at the end of 2024 which showed that only 5% of staff use sustainable and active travel (3,138 respondents). Travel questions will be included in the surveys every other quarter.
Since Easter 2024, we have established regular bank holiday switch off campaigns to raise awareness of energy efficiency. During Easter 2024 bank holiday, we made 3% cost savings in electricity despite increased tariff cost since 2023 and a 13% reduction in consumption. A switch-off campaign did not take place over the early May Bank Holiday, over the late May Bank Holiday switch-off we reduced electricity consumption by 13%. The August bank holiday switch-off saw a 35% reduction in energy consumption resulting in £4,488 of savings. The Christmas and new year switch-off saw a 7% reduction in electricity consumption and a cost saving of £4,182.
We have developed an East24 intranet page focused on sustainability with monthly waste updates, sustainable estates, fleet Trust-procured fuel emissions, Entonox emissions, links to the greener NHS website and more.
Since September 2024, the sustainability team has presented a 10–15-minute slot in monthly staff inductions. This ensured that sustainability was promoted to all new staff, through introducing the NHS net zero targets, waste management and sustainable commuting.
EEAST is leading the sector with two clinical engineering and one Emergency Operations Centre staff in the first cohort of a new 15-month sustainability apprenticeship (Sustainable Healthcare Academy) via LDN Apprenticeships (started September 2024). The sustainability team liaised closely with LDN Apprenticeships to hold an insight session exclusively for Trust staff and to work together to give potential apprentices the knowledge they needed to make an informed decision whether this was the right path for them. There was also an ambulance service only insight session which was arranged after the Trust sustainability team introduced the green environmental ambulance network (GrEAN) to the new apprenticeship and spoke with colleagues at LDN Apprenticeships to inform staff within the network about the opportunity.
Estate Improvements
We continued to improve the energy efficiency and sustainability of our estate via our capital investment programme. Key projects that took place during 2024/25 include:
- Whole building refurbishments included upgrading insulation, heating controls and new LED lighting with controls in Thetford and Ampthill.
- LED lighting installed across all six counties with 95% of Trust sites covered, some include controls such as motion sensors.
- We continued to improve the facilities for our workforce to benefit wellbeing and diversity. A multi-use wellbeing and multifaith room was installed at King’s Lynn, Chelmsford Lawnside, Stevenage and March.
- Garage heaters were replaced with more efficient systems at Huntingdon, March, Waveney and Cambridge.
- Replaced single glazed windows at Saffron Waldon, Swaffham and Fakenham with A+ rated double glazed versions.
- Solar PV panels to generate electricity along with battery storage were installed at Waveney and Chelmsford EOC. Additional battery storage was installed at Peterborough, Melbourn, Welwyn Garden City and Cromer, and additional PV was installed at Hellesdon EOC.
- Efficient boilers were installed at Hellesdon EOC. The oil-fired heating system at Saxmundham was replaced with a more efficient and lower carbon natural gas boiler.
Bury St Edmunds Hub
The Bury St Edmunds Hub was officially opened on 27 September 2024 and is our first site to achieve the independent environmental assessment BREEAM Excellent. The site has no mains gas supply (using air source heat pumps for heating and hot water), solar PV, covered cycling parking, planting uses native species, wellbeing garden and EV charging bays.
Staff wellbeing is at the heart of the design. The building includes a quiet room, a multi-faith room, a nursing room, a gym and outside wellbeing spaces for relaxation and exercise.
Ipswich Hub
Construction of the new Ipswich Hub continues. The building is watertight and nearing first fix stage.
We have received additional funding approval from the National Energy Efficiency Fund (NEEF) for £138,407 for LED lighting and £108,986 for solar PV panels.
Carbon Footprint
Our strategy to meet net zero is detailed in our 2021-2026 Green Plan which is available on our website under our corporate strategy. In line with other NHS organisations and our legal commitment outlined in the Health and Care Act 2022, the Trust is committed to reaching net zero greenhouse gas emissions for those emissions we can control by 2040 and for those emissions we can influence by 2045.
The NHS baseline year for our net zero targets is 2019/20 (as we do not have data going back to 1990). This means that the 80% target as stated in Delivering a Net Zero NHS equates to a 47% reduction between 2028-2032. We have set an organisational target to reduce absolute emissions we can control by 50% by 2030 (using a 2019/20 baseline). Emissions are measured in tonnes of carbon dioxide equivalent (tCO2e) which provides a common measurement encompassing all greenhouse gases.
We continued to improve the data acquisition, analysis and reporting of our carbon footprint. We have significant gaps in Trust-derived data, including hybrid working, non-telematics fleet, business travel, staff commuting, supply chain and medicines. This means that we cannot currently provide a full footprint of our directly controlled emissions (NHS Carbon Footprint) and emissions we can influence (NHS Carbon Footprint Plus).
We regularly monitor direct emissions from Trust-procured fuel for fleet vehicles (our single biggest source of direct emissions), energy consumption and Entonox (nitrous oxide) usage, although we are working on improving the accuracy of this data.
Fleet Fuel Emissions
Due to increasing vehicle numbers to fulfil national response targets, our Trust-procured fuel emissions from bunkered fuel stores and fuel cards for 2024/25 have increased to 16,312 tCO2e, 1.2% above 2023/24 levels (22% below 2019/20 baseline, target is 25% below baseline or 15,650 tCO2e, so off track for net zero by 2040). This is the first year we have not met the net zero trajectory for fleet emissions. As fleet fuel consumption makes up our largest single source of emissions, this is a priority area for meeting our net zero ambitions.
We estimate that our fleet emissions make up between 40-85% of our direct carbon footprint. The reason for this uncertainty is because we have significant gaps in data to produce our full fleet emissions footprint and have limited business travel data, particularly for business travel submitted through expenses. Due to the significance of this emissions source and continued reporting requirements via the Greener NHS Transport Data Collection (ambulance trusts were required to submit data from 2022/23), we aim to increase our data acquisition and analysis.
Energy Emissions
Almost all electricity and gas meters have half-hourly automatic smart meters which ensures more accurate billing. The Trust is also ensuring that all solar PV installations are connected to a central platform to access real-time electricity generation data to quantify energy, cost and carbon savings made monthly. The sustainability team have conducted energy audits at 13 high energy consuming sites to identify potential energy savings projects for our capital programme or for behaviour change campaigns.
Overall, 2024/25 energy emissions are 6% above the previous year, with a 2% decrease in electricity and 13% increase in gas. Emissions at 2,962 tCO2e are 13% below the 2019/20 baseline, so we are off track for net zero by 2040 (the 2024/25 target was 25% reduction or 2,542 tCO2e).
Entonox (nitrous oxide) Emissions
We receive monthly Entonox usage data from our supplier which enabled us to measure our nitrous oxide emissions (which totalled 1,403 tCO2e in 2024/25). This was an 8% reduction compared with last financial year and a 33% reduction since the 2019/20 baseline, meaning we are well on track for net zero emissions by 2040. It must be noted that we do not have accurate data on our clinical usage versus waste, which the College of Paramedics has found represents 25% by volume.
Anaesthetic gases, such as mixed nitrous oxide, are being targeted as a priority area for emissions reductions by the NHS as they are extremely potent greenhouse gases (nitrous oxide is 265 times more potent than carbon dioxide at trapping heat in the atmosphere).
Clinicians currently rely on the fill gauge on cylinders showing red before switching cylinders. Across the sector, this practice leads to an estimated 25% remaining in mixed nitrous oxide cylinders returned to suppliers as waste. Suppliers are required to vent any remaining gas to atmosphere prior to refilling cylinders. We aim to investigate waste reduction techniques, such as an app available via our supplier which monitors usage or through developing clinical guidance.
Medicines Management have been trialling Penthrox as an alternative analgesic in Norfolk and Waveney from April 2024. Life cycle analysis shows that Penthrox has a significantly lower climate change impact when compared with nitrous oxide (the active ingredient, methoxyflurane, is 4 times more potent than carbon dioxide at trapping heat in the atmosphere).
Electric Vehicle Infrastructure
The Trust has purchased 27 dual 40kW DC electric vehicle chargers and is working with UK Power Networks to get these installed onto sites. We are awaiting delivery of 30 dual 22kW and 35 dual 7.4kW AC chargers which will be installed throughout the East of England following site electrical surveys and discussions with fleet and operations departments. We have also purchased a back-office charge point management system to support the EV infrastructure transformation.
Fleet Electrification
A working group to develop the Trust’s fleet electrification strategic plan was launched on 26 February 2025 which will follow the NHS Net Zero travel and transport strategy roadmap. Four key areas have been identified, and senior responsible officers for each area will be accountable for delivering the work plan:
- Developing our infrastructure
- Preparing our people
- Replacing our vehicles
- Deploying our vehicles
We continued to add electric vehicles to our fleet following the successful trials of response vehicles in 2022/23. In 2024/25, 12 Mercedes eVito mental health response vehicles (MHRVs) and 15 Skoda Enyaq rapid response vehicles (RRV) entered service.
We continued to replace the inefficient Mercedes DSA with alternative DSA-type vehicles, including Renault, MAN and Ford.
Purchasing
All Trust tenders included a minimum 10% weighting criteria for social value and net zero with tenders above £5 million including the requirement for suppliers to publish a carbon reduction plan in line with legal requirements and in support of our sustainability strategy.
The Trust updated its modern slavery statement in line with the ethical trading initiative-modern slavery statement evaluation framework and in line with best practice.
Trust tenders support our Net Zero and sustainability aims through:
- Use of the supplier sustainability agreement as a pass or fail element within FTS tenders.
- Use of the Standard SQ which includes as pass or fail elements for carbon reduction; equality, diversity, and inclusion; as well as modern slavery.
- Use of three clear areas of evaluation that include quality, social value and sustainability (minimum 10%) as well as commercial weightings.
The procurement department has contracted the social value portal to develop the Trust’s social value framework following local needs analysis and a series of Trust-wide collaborative workshops to agree themes outcomes and measures.
A social value and sustainable procurement policy is being developed. The new PPN002 social value model requirements published in February 2025 will be incorporated into this policy.
Many estates and facilities contracts are due for renewal and will be reviewed as per our carbon reduction plan and social value requirements. We purchased 100% recycled, FSC and EU Ecolabel accredited paper and double-sided printing is the default option on all our printers. We signed the plastics pledge, and all staff were issued with reusable water bottles, and the heatwave plan has been adjusted to only supply bottled water during protracted or remote incidents.
Resource Optimisation
Across the Trust’s various departments, teams are collaborating to be more sustainable and efficient in the way they work.
Initiatives from Stores
- Switched to a screen wash manufactured from alcohol hand gel (this was an innovative way to reuse excess hand gel produced during COVID).
- Stores have changed aerosol devices to liquid sprays to remove fluorinated greenhouse gases.
- They are reusing packaging and cardboard boxes rather than disposing of them. New bins to collect cardboard for recycling were introduced at Hellesdon EOC and Letchworth sites. We engaged with our supplier (NHS Supply Chain) to reduce packaging and use of plastic bags.
- To reduce waste and out-of-date stock, Stores no longer hold excess stock.
- To reduce mileage and carbon emissions from deliveries, they use fewer suppliers for purchasing items. Stores have economical vehicles that are lightweight and can carry a large load.
Processes
- People services have moved all paper payslips to electronic in 2024 and are in the process of doing the same with HR forms and personnel files. The electronic HR forms build is now completed with local testing planned. Once the local testing has been completed, a rework phase will occur to make amendments. The system should be live for a pilot in April 2025. All forms are currently being digitalised.
- We have surveyed each site to determine the utilisation of space, and the Asset Booker app is now live for three sites for hot desks and meeting rooms with more sites being added over time.
- As part of the NHS People Promise, the Trust offers flexible working arrangements. This has a benefit on the health and wellbeing of staff and on our Trust carbon footprint by reducing staff commuting and site energy consumption.
Equipment
- Returning Trust property is a priority area, with a task and finish group established to alter new starter contracts, place HR3 form reminders on managers checklist, devise a communications plan and organise a series of IT amnesty campaigns, with October 2024 promoted as IT Amnesty Month. In the first amnesty, 82 items were returned with 32 being able to be reused which had a total value of £11,300. • A uniform task and finish group was established in September 2024 to determine efficient and sustainable procedures for the issue and disposal of uniform. One of the main aims is to introduce a system for re-using uniform as opposed to the current practice of secure disposal, which will save costs and optimise resources.
Waste Management
In January 2024, the Trust introduced an offensive waste stream to clinical waste to save costs and reduce the environmental impact of incinerating clinical waste. The Trust met the national target of 60% in July/August 2024, as expected. Since then, the offensive waste stream has continued to increase to over 70%.
Members of the sustainability team accompanied the facilities manager on various duty of care visits to our waste contractors. We visited the clinical waste Sharpsmart facility in Rainham to see how our bagged clinical waste is processed. We also visited Rookery South which is where Veolia take our general waste to incinerate it to produce energy, meaning that none of our general waste goes to landfill. We also visited the ShredStation facility in Norwich where our confidential paper waste is shredded before the material is delivered to a paper mill to make recycled paper. After uniform is shredded, depending on the fibres and the quality of the uniform, the materials are either recycled into underlay for carpets and cushions or it is incinerated through waste to energy recovery. These visits are always valuable to understand the processes that occur after our waste is taken from sites.
The sustainability team is working with the facilties manager and site contacts to improve segregation and recycling rates at targeted sites. Cromer Ambulance Station was selected for a visit as it had a recycling rate less 10% in April 2024. The site visit included engaging with the Local Operations Manager (LOM) to set out next steps to increase this and now, Cromer is a consistent top 10 performer and their recycling rate is always above the Trust average (25%) and averages at 40%. Members of the Sustainability Team have also engaged with the three EOCs, as these large sites had below average recycling rates. Recycling rates in EOCs are now all above the Trust average of 25%.
Within the Sustainability Pilot Site Project, three of the sites aim improve their recycling rates. One site that has seen success within this project is Peterborough which is one of our largest sites and had a recycling rate below the Trust average. Green Champions and the Sustainability Team worked together to ensure the correct bin bags were placed in bins and to put waste segregation posters next to all bins on site. The recycling rate has been slowly increasing and is now above the Trust average.
Wellbeing Gardens and Biodiversity
We are piloting an initiative at Longwater to bring in community gardening groups to maintain our wellbeing gardens. Costessey Community Gardening Club are currently visiting the site once a month, but this will increase to two visits a month in the spring.
Wellbeing gardens provide a green space for staff to decompress and take time for themselves in amongst the challenging and traumatic times they may face in their role. These spaces are crucial for staff wellbeing and offer a space to improve biodiversity across the Trust with different species of trees, plants, bug hotels and bird feeders. The Trust has 13 wellbeing gardens with plans to have more at sites including Southend and Peterborough.
The sustainability team coordinated the Trust’s first tree planting programme. A total of 420 trees from NHS Forest plus 5 donated trees from a member of staff making a grand total of 425 trees were planted by the end of the 2024/25 planting season, the most of any UK ambulance service! The first 20 trees for an orchard were planted in Hellesdon in November 2024. A hedge of 180 trees was planted in Hellesdon along with five oak trees in January 2025. In March 2025, 20 trees were planted at Potter Heigham, 20 fruit trees for Chelmsford Lawnside and a hedge of 180 trees planted at Cromer.
Looking Forward
Our Green Plan 2021-26 will be reviewed and refreshed in line with the national guidance by July 2025. A task and finish group will be established to devise our next Green Plan for 2026, which will incorporate our Travel Plan.
We plan to conduct energy audits of all sites to enable us to meet our 2025/26 strategic objective of at least a 5% saving on energy consumption in line with the Productivity Mission of the Trust Strategy 2025-30.
We are part of an NHS England trial of electric DSAs, with the first 3 Ford E-Transit vehicles due for conversion and delivery in summer 2025. In line with the NHS Travel and Transport strategy, we will be installing EV chargers at hub sites to be able to support our growing fleet of electric RRVs, MHRVs and the incoming electric DSAs.
After a successful pilot working with Costessey Community Gardening Club, we have begun contacting more community groups for other sites with wellbeing gardens in need of care.
As a part of the sustainability pilot site project, Southend, Cambridge and Peterborough are planning to turn an area of their site into a wellbeing garden. The sustainability team will work with green champions and staff on site alongside the Trust Charity and wellbeing department to ensure the space is used effectively with staff in mind.
After a successful 2024/25 planting season, planning has already begun with 6 sites expressing interest in planting trees and hedges at their site. Initial surveys will be done on these sites in the summer and autumn before the 2025/26 season begins at the end of November. We have set a target to plant at least 500 trees next financial year.
There are plans to install solar PV and battery storage at nine sites around the Trust to help reduce electricity bills to save money and become more self-sufficient.
The sustainability team will work with the facilities manager to look at large sites with low recycling rates and engage with staff and green champions on the site to increase these recycling rates. By focusing on larger sites, we will be targeting those sites with the largest impact on our overall recycling rate. The main reason behind this is that 12 of our sites produce over 40% of the Trust’s waste so if these sites and staff can be influenced, then we should see a significant increase in Trust recycling rates.
A task and finish group was set up in 2024/25 to look at how uniform can be reused through a central uniform store with laundering to help reduce waste via our confidential waste contract, as well as save purchasing costs. This initiative will continue in 2025/26.
The sustainability team will increase awareness of sustainability and climate change by growing the green champions network and by visiting sites to speak to staff and gather feedback about sustainability. Feedback from site visits in 2024/25 has been positive, so we will continue to develop our staff engagement initiatives.
Task Force on Climate-related Financial Disclosures (TCFD)
The GAM has adopted a phased approach to incorporating the TCFD recommended disclosures as part of sustainability annual reporting requirements for NHS bodies, stemming from HM Treasury's TCFD aligned disclosure guidance for public sector annual reports. TCFD recommended disclosures as interpreted and adapted for the public sector by the HM Treasury TCFD aligned disclosure application guidance, will be implemented in sustainability reporting requirements on a phased basis up to the 2025-26 financial year. Local NHS bodies are not required to disclose scope 1, 2 and 3 greenhouse gas emissions under TCFD requirements as these are computed nationally by NHS England.
The phased approach incorporates the disclosure requirements of the governance, risk management and metrics and targets pillars for 2024-25. These disclosures are provided below with appropriate cross referencing to relevant information elsewhere in the ARA and in other external publications.
Governance
Board oversight of climate-related issues
The East of England Ambulance Service NHS Trust has plans in place which take account of the ‘Delivering a Net Zero National Health Service’ report under the Greener NHS programme. The Trust ensures that its obligations under the Health and Care Act 2022 relating to the Climate Change Act 2008, Environment Act 2021 and climate change adaptation requirements are met.
The Trust has clear governance structures to support climate and sustainability reporting and assurance. One of the Trust’s four strategic goals detailed in the Corporate Strategy 2020-25 is to be an environmentally and financially sustainable organisation with a related strategic risk (SR4) being overseen by the Board devolved authority Compliance and Risk Group.
The Trust’s Sustainability Enabling Strategy 2020-25 and Green Plan 2021-26 are underpinned by robust objectives. The Green Plan was approved by the Trust Board in November 2021. The Strategy sets out how the Trust will govern, manage and implement its Sustainability Plans for the 5-year period 2020-2025 and supports the Corporate Strategy approved by the Trust’s Board of Directors.
Assurance and reporting for sustainability issues including climate action and goals is delivered through robust governance assurance processes. The Trust has a designated Board member champion who is responsible for the delivery of the sustainability agenda.
Sustainability agenda assurance is supported by internal audit, monthly integrated performance and Board assurance framework reporting, and an annual report submitted to Board. The Board receive sustainability updates via the CEO report at each bimonthly Board meeting. This report contains progress reports for key scope 1 and 2 emission sources (see Section 5) mapped against the Trust’s net zero pathways as set out in the Green Plan.
Management's role in assessing and managing climate-related issues
The Environment and Sustainability Manager coordinates workstreams and monitors progress against targets, providing assurance reports to internal and external stakeholders. The bi-monthly Sustainability Working Group, responsible for the functional delivery of the Strategy and Green Plan, reports to the Board via the monthly Compliance and Risk Group with an escalation process to the Executive Leadership Team and from there to the Board. As of November 2024, the Environment and Sustainability Manager became a member of the bi-monthly Finance and Sustainability Committee which has a direct reporting line to the Board, improving the accountability and governance of the Green Plan.
The Executive Clinical Group supports the delivery and takes decisions to deliver the strategic objectives of the Trust. In undertaking its role, the Executive Clinical Group takes business as usual and strategic decisions to deliver its ultimate purpose.
The Transformation Programme Group is responsible for ensuring connected planning principles are applied to any proposed programmes or initiatives and sustainability is a key consideration in the business case template:
Sustainability - How will the project affect Trust sustainability including environmental considerations, efficiencies, product lifecycles, energy use, community engagement and so on? Include the carbon impact if relevant.
The Trust has established a programme of themed Accountability Forums, which provide an opportunity for each department and sector to consider its areas of delivery, identifying themes for improvement and considering sustainability and climate matters.
Risk Management
Our processes for identifying and assessing climate-related risks
The Trust’s approach to identifying and assessing risk is set out in the Risk Management Strategy and Policy:
The Trust will identify its significant risks from the following sources .
- The investigation of incidents, claims, and complaints.
- Concerns and complaints raised by stakeholders, patients and staff.
- Expertise of managers and other lead personnel.
- Issues raised by Trust committees and groups.
- External organisation reports and inspections.
- External, internal and clinical audits and surveys.
- Carrying out risk analyses or assessment work.
- And any other relevant information.
The following factors will be taken into account when the risk is analysed:
- The full extent of the consequences of the risk.
- The likelihood of the risk occurring.
- Any means by which the risk is currently controlled or mitigated.
- How the Trust will be assured that the risk is being adequately managed.
- Developing further mitigating controls/accepting the risk.
Following analysis of the risk, the risk lead, in conjunction with other relevant people inside or outside the Trust, will consider the circumstances identified and decide whether further mitigating controls are necessary.
The Trust’s Sustainability Team work with external experts including ICB partners and the Centre for Sustainable Healthcare to progress our understanding of environmental risks affecting healthcare establishments.
The Environment and Sustainability Manager is working with the Risk Manager to add climate-related risks to the Trust risk register. Recommendations were made at the February 2025 Finance and Sustainability Committee meeting to add climate change and sustainability risks to the Board Assurance Framework (BAF). At the March 2025 Trust Board meeting, members agreed to suspend the BAF whilst this is aligned to the new strategic direction following publication of the Trust Strategy 2025-30. The new BAF is likely to be released in June 2025.
Table 1: Climate-related risks on the Trust Risk Register
| Risk category and ref | Risk | Residual score | Mitigations and controls |
|---|---|---|---|
| Strategic Risk (STR0005) | SR4: If we do not resolve long standing organisational inefficiencies, we will be unable to deliver an effective, sustainable, value for money service to public. | 12 I (4),L (3) | QCIP programme, leadership and governance infrastructure Sustainability and Green Plan with KPIs monitored |
| Strategic Planning (SP0002) | Risk that inadequate climate change mitigation and adaptation will compromise the services we deliver to the public. | 16 I (4),L (4) | Trust Green Plan Winter Plan and Adverse Weather Cards Monitoring and reporting progress on Green Plan to stakeholders Energy auditing programme and capital programme Business Continuity Plans |
| EPRR and Specialist Operations (EPR0001) | If the Trust fails to comply with the Civil Contingencies Act 2004, the NHS Act 2006 and the Health and Care Act 2022 then the Trust will be in breach of legislation and its statutory obligations as a Category 1 responder. | 15 I (5),L (3) | Engagement by EEAST at local resilience fora Business Continuity Plans Annual Trust wide business continuity management exercises Winter Plan and Adverse Weather Cards |
| Estates (EST0004) | IF we do not install EV infrastructure THEN we will not be ready for the phase out of diesel and petrol vehicles RESULTING IN the Trust not being able to comply with our statutory accident and emergency service. | 12 I (3),L (4) | Liaison with UK Power Networks regarding EV infrastructure installations EV infrastructure consultant EV charge point management system Dynamic load balancing required Fleet Electrification Plan (in development) |
Our processes for managing climate-related risks
Risks identified by the organisation which require management are added to a risk register. Managers are responsible for managing risks which impact their objectives within the organisation. The risk register assesses and scores the risk based on the likelihood and impact (1-5, with the highest risk score of 25). Each risk must have controls identified and planned steps to reduce the risk score associated wherever possible.
Risk registers are carefully managed within the organisation. Risks rated 1 to 12 should be managed at directory/sector level and held on the Directory Risk Register. Risks rated 12 to 15 should be reported to the Deputy Director, Head or Service Manager, and the Director should be made aware with risks held on the Corporate Risk Register. Risks rated above 15 should be reported to the Director immediately and the Board made aware; it should be considered whether these should be escalated to the BAF if the risk impact will be experienced in more than one directorate/sector.
Oversight of the risk register is held by the appropriate Deputy Director or Head of Department and are reviewed and at all team meetings. Moderate risks (rated 8 to 12) are presented for oversight at relevant governance groups. The Sustainability Working Group is the governance group responsible for oversight of climate-related and sustainability risks. High risks (rated 15 to 25) are presented for challenge and assurance and at the monthly Compliance and Risk Group with an escalation process to the Executive Leadership Team.
The Sustainability Team identifies risks associated with the delivery of the Green Plan and maintaining compliance with environmental legislation. These risks are most closely aligned to mitigation risks pertaining to the climate. Secondly, the risks of short-term extreme weather events, especially flooding and heatwave, are identified within the Emergency Preparedness Resilience and Response risk register. These climate-adaptation risks have been identified as enduring and ongoing. The Trust has limited ability to tackle the root cause of these risks and so the risk is managed within our preparedness and business continuity processes.
We are planning a comprehensive review of climate-related risks on our risk register, with climate change and sustainability-related risks added to the BAF with specific climate risks identified which acutely impact service areas/localities placed on the Directory Risk Registers and the Corporate Risk Register.
How processes for identifying, assessing and managing climate-related risks are integrated into our overall risk management approach
The Trust manages climate-related risks and issues in much the same way as any other risks or issues, as set out in the Risk Management Strategy and Policy.
Metrics and Target
The metrics we use to assess climate-related risks and opportunities in line with our strategy and risk management process.
The Trust produces a dashboard report (Integrated Performance Report) which is reviewed monthly by the Executive Leadership Team (ELT). This dashboard contains metrics that connect to climate-related risks:
- Purchased electricity, natural gas and water consumption per square metre (kWh/m2).
- Combined utilities emissions per square metre (kgCO2e/m2)
- Average miles per litre of fleet fuel
The Trust holds a regular Accountability Forum led by a panel of senior leaders to provide assurance to ELT. At the second Estates Forum held on 1/11/24, Sustainability was a key focus for the meeting. The Forum requested data and timeframes on how we could achieve net zero targets, particularly for fleet.
As an NHS organisation we are not required to disclose or develop processes to disclose scope 1, scope 2 and scope 3 emissions. Emissions estimates for NHS England are provided by NHS England. However, as a Trust we continue to improve the data acquisition, analysis and reporting of our emissions. We have significant gaps in Trust-derived data, including hybrid working, non-telematics fleet, business travel, staff commuting, supply chain and medicines.
The targets we use to manage climate-related risks and opportunities and performance against targets
In line with other NHS organisations and our legal commitment outlined in the Health and Care Act 2022, the Trust is committed to reaching net zero greenhouse gas emissions for those emissions we can control by 2040 and for those emissions we can influence by 2045. We have set an organisational target to reduce absolute emissions we can control by 50% by 2030 (using a 2019/20 baseline). Each month the Trust monitors and has set annual absolute emission targets for our three largest emission sources (see Section 5):
- Fleet emissions (Trust-procured fuel)
- Purchased electricity and natural gas emissions
- Nitrous oxide emissions from Entonox consumption
Developing the strategy
As a health care provider, we operate in a context of ever-changing needs. We know that by 2040, a third of people in the east of England will be over 60, and many of these people live in rural or coastal areas. With more patients having more complex needs and living in harder to reach locations this will increase demand for our services. This is not just a challenging future we must prepare for - it is a reality that already impacts our service. So, even with the improvements we’ve made in recent years, we recognise the need to continue to evolve how we deliver our service to respond effectively to the needs of our communities in the east of England.
As highlighted in last year’s report, EEAST sought to address these challenges, through the introduction of a Clinical Strategy 2023-26, this document sat alongside the People and the Sustainability Strategies. The organisation still however lacked a single coherent narrative that would tie the three strands together.
We are pleased to say that the EEAST Strategy 2025-30 was launched in May 2025. The strategic framework developed not only provides a new vision for our future but outlines the missions, values and behaviours required to get us there. We’re excited about the improvement journey we’re on, and how this strategy sets our path for the next five years. It is important to highlight too that this ambition was designed by our people, patients and partners, following EEAST’s most significant engagement programme to date.
Developing the strategy
The development of our new Trust strategy took place over three phases, namely:
- Diagnose and Forecast
- Define options and prioritise
- Deliver and evolve
Phase 1: A full review of our policies, performance and health data, as well as stakeholder insights to tell us what was changing. We reviewed our policies, our Trust performance between 2020 and 2025, and health and demographic data for the east of England. Looking at these together, we produced insights into the nature and location of services that EEAST delivers. This gave us evidence about the increasing complexity we face in responding to an ageing population, living at the edges of our region. This has led us to focus on:
- Working together with our partners to enhance performance and improve patient outcomes.
- Tailoring care to the conditions our patients need an emergency response to.
- The role of Hear & Treat and our approach to delivering this.
- Culture, values and productivity.
- The role of technology in innovating our processes.
Phase 2: Our online engagement programme to hear from our people, patients and partners We used this analysis to create four big questions. These were then posed to our people, patients and partners over a six-month period. Questions explored what it means to be an ambulance service and what we can do to improve. We also looked at what it’s like to work at EEAST and how we treat one another. We received more than 12,000 ideas, comments and votes from 2,042 people using an online moderated platform. We used these insights to develop the EEAST Strategy 2025-30. What we heard:
- We need a clear purpose and vision of the future with everyone pulling in the same direction, with clearly defined partnerships and measurable outcomes.
- We need to make achieving our goals everyone’s job.
- We need everyone to embrace continuous learning and new ways of doing things.
- We need clear and shared behavioural expectations.
- We need clear plans to deliver.
Phase 3: Consisted of the write-up and communication of the EEAST Strategy 2025-30 The Trust Values and Behaviours, and the Trust Strategy were shared at EEAST leadership development days in September 2024 and April 2025 respectively. The final version of the strategy document was launched in May 2025.
The EEAST Strategic Framework
The EEAST Strategy 2025-30 talks to saving lives, investing in people and working with partners. The framework outlined below talks to the intended direction of the organisation, what needs to be done in the next five years in order to reach our destination, and what values and behaviours will support us along the way.
Why we're here
Our direction is defined by our purpose and vision
Our purpose:
We care for our patients, our communities and each other, making every minute count to save lives and improve outcomes for patients.
Our vision for our region:
Everyone in the east of England will have high-quality, urgent and emergency care. Heath and care providers across the region will work in partnership with the East of England Ambulance Service to make this happen.
What we'll achieve over the next five years
Our four missions
Our Patient mission:
To provide high quality urgent and emergency care that is fair, responsive and focused on patient need.
Our People mission:
To provide a supportive, inclusive, and empowering environment for our people. It will support individual and organisational performance.
Our Partnership mission:
To connect patients to the best care, at the right time, first time, every time, through working with our partners.
Our Productivity mission:
To be an innovative, efficient, and sustainable healthcare partner. We will meet the needs of our communities within the resources available to us.
Values and Behaviours
We are accountable
- I am honest and do what I say I will do.
- I collaborate to get the job done well.
- I take responsibility for my own wellbeing and actions.
We are respectful
- I am inclusive.
- I am empathetic.
- I am compassionate.
We strive to be excellent
- I develop the skills I need to do my job well.
- I act on feedback.
- I keep improving the way we work.
Continuous Evolution
To achieve our vision, we must have effective processes and approaches to how we run our organisation.
Effective planning: how we organise our planning and investments to deliver our aims.
- We will align everything we do with delivering our missions within the resources we have. For example, how we can use our estate to deliver patient care more effectively. It will enable us to work better as multi-disciplinary teams focused on outcomes.
Organisational and personal governance: how we hold ourselves to account as individuals and as an organisation.
- Our purpose, vision, missions and values will guide our actions, at all levels. Our governance framework will support us to ensure everything we do helps to achieve our missions, and that we deliver what we say we’ll deliver.
Designing and delivering change: how we improve the way we deliver services to patients and how we run our business.
• We will capture insights from our patients, people and partners and involve them in delivering change. We will use technology to work and innovate better and to deliver and embed change.
Next steps
While we are excited at the prospect of embarking on this new journey, the hallmark of any good strategy is to make certain that the actions the organisation will take are aligned to the intended direction of the strategy. To this end, we will look to expand our four missions and develop an operating model that will give us the best chance at success.
I confirm that this performance report complies with the reporting requirements.
Neill Moloney, Chief Executive Officer, June 2025
Directors Report
The Board
Our Board of Directors met in public on six occasions between 01 April 2024 and 31 March 2025 with all meetings being quorate. No scheduled meetings were stood down during the year. The Board met in private ten times to discuss confidential matters; all decisions made were reported to the in public Board meeting. Extraordinary meetings were held to approve the Annual Report and Accounts, and an Annual General Meeting was held in September 2024.
Our Trust Board voting members consist of our Chair, five Non-Executive Directors, the CEO and four Executive Director members, as the corporate decision-making body of the Trust. Accountable for all strategic, operational, and financial decision-making, the Board has powers to delegate and decide to exercise any of its appropriate functions through a sub-Committee. Our Board was supported by two non-voting Executive Directors and three Associate Non-Executive Directors during the year.
The Chair is responsible for ensuring the Board of Directors focus on the strategic development of the Trust and that robust governance and accountability arrangements are in place. We are required by the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 to ensure that our directors are fit and proper for their roles. To fulfil this responsibility, the Trust has undertaken appropriate Fit and Proper Persons checks for all directors during 2024-25.
The Trust had a new Chief Executive Officer formally taking over accounting officer responsibilities from September 2024. Also, there were changes to the following executive roles: Chief of Clinical Operations (the role is currently covered on interim basis), Director of Corporate Affairs and Performance (the role is currently vacant and being reviewed), Director of Integration (the executive role has been dissolved with its portfolios absorbed by other directorates).
Board Sub-committees
The Board delegated certain powers to our sub-Committees, except for executive powers, and each of these sub-Committees was chaired by a Non-Executive Director, working in conjunction with a lead Executive Director, reporting directly into the Board providing assurance over key matters. They also escalated emerging issues for the Board's attention.
The Board has established six sub-Committees which worked together to support cross-reporting and consideration of assurance to support the Board by: Providing advice on strategic development and performance within terms of reference.
- Gaining assurance and providing oversight on key aspects of strategic goals
- Undertaking specific responsibilities as approved by the Board
Each sub-Committee had formal terms of reference, approved by the Board and set out in the Standing Orders, establishing the roles and responsibilities of our sub-Committees. The terms of reference were reviewed as part of a formal annual Committee effectiveness review with recommendations for areas for development being approved by the Board. Each sub-Committee had a business planner to help direct the focus of assurance.
Audit and Risk Committee
The audit and Risk Committee provided the Board with a means of independent and objective review of financial and corporate governance, internal control, assurance processes and risk management across the whole of the Trust’s activities both generally and in support of the Annual Governance Statement. Membership and attendance
- George Lynn (Chair), Non-Executive Director (4 of 5)
- Chris Brook, Non-Executive Director (2 of 5)
- Omid Shiraji, Associate Non-Executive Director (4 of 5)
- Victoria Corbishley, Associate Non-Executive Director (1 of 1)
The Director of Finance is a standing attendee at the Audit Committee. All other Non-Executive Directors (excluding the Chairman) are invited to attend as are the External Auditors, Internal Auditors and Counter Fraud Lead. Other Executive Directors, including the CEO and other senior managers of the Trust are regularly invited to attend meetings of the Audit Committee for specific items.
Nominations, Remuneration and Terms of Service Committee
The Nominations, Remuneration and Terms of Service committee determined appropriate remuneration and terms of service for the Chief Executive and other Executive Directors and regularly reviewed the structure, size and composition (including the skills, knowledge and experience) required of the Board and made recommendations to the Board or NHSE as appropriate, about any changes.
Membership and attendance
- Catherine Glickman (Chair), Non-Executive Director (6 of 6)
- Mrunal Sisodia, Non-Executive Director, Trust Chair (3 of 6)
- Wendy Thomas, Non-Executive Director (4 of 6)
- Julie Thallon, Non-Executive Director (4 of 6)
- George Lynn, Non-Executive Director (1 of 6)
- Chris Brook, Non-Executive Director (1 of 6)
- Omid Shiraji, Associate Non-Executive Director (5 of 6)
Quality Governance Committee
The Quality Governance Committee provided assurance to the Board that there was an effective system of quality governance and internal control across clinical activities to ensure patients are treated with compassion, dignity and respect. Provided assurance that the essential standards of quality and safety are being delivered by the Trust. Also provided assurance that the processes for the governance of quality are embedded throughout the organisation to improve the experience of patients.
Membership and attendance
- Catherine Glickman, Non-Executive Director (Chair) (5 of 5)
- Wendy Thomas, Non-Executive Director (5 of 5)
- Julie Thallon, Non-Executive Director (4 of 5)
- Victoria Corbishley, Associate Non-Executive Director (5 of 5)
- Omid Shiraji, Associate Non-Executive Director 4 of 5)
- Melissa Dowdeswell, Chief of Clinical Operations (2 of 4)
- Simon Chase, Chief Allied Health Professional / Director of Quality (5 of 5)
- Simon Walsh, Medical Director (4 of 5)
The Chairman, Chief Executive and all other Non-Executive Directors are invited to attend, and other Executive Directors, senior managers, and health professional staff attend for specific items.
Finance and Sustainability Committee
The Finance and Sustainability Committee provided assurance to the Board that financial performance was delivered in accordance with the agreed strategy, plans and trajectories. Providing assurance on the delivery and performance of the sustainability strategy also overview and scrutiny in any areas of finance and sustainability referred to it by the Board.
Membership and attendance
- Chris Brook (Chair), Non-Executive Director (5 of 6)
- Julie Thallon, Non-Executive Director (6 of 6)
- Omid Shiraji, Associate Non-Executive Director (3 of 6)
- Kiran Mahil, Associate Non-Executive Director (0 of 0)
- Kevin Smith, Director of Finance (6 of 6)
- Kate Vaughton, Director of Integration (1 of 2)
Other members of staff are invited to attend as required.
Performance Committee
The Performance Committee provided assurance to the Board that operational performance was delivered in accordance with the agreed strategy, plans and trajectories. It provided overview and scrutiny in any areas of operational performance referred to it by the Board.
Membership and attendance
- Julie Thallon (Chair), Non-Executive Director (4 of 5)
- Wendy Thomas, Non-Executive Director (5 of 5)
- George Lynn, Non-Executive Director (3 of 5)
- Chris Brook, Non-Executive Director (1 of 5)
- Melissa Dowdeswell, Chief of Clinical Operations (4 of 4)
- Kate Vaughton, Director of Integration (1 of 2)
- Darren Meads, Interim Chief of Clinical Operations (1 of 1)
The Chairman, Chief Executive Officer and Non-Executive Directors are invited to attend. Other Trust Directors and managers and health professional staff attend for specific items.
People Committee
The People Committee provided assurance to the Board on the quality and impact of the people strategy and the effectiveness of people management in the Trust. This included but was not limited to recruitment and retention, training, appraisals, employee health and wellbeing, learning and development, employee engagement, reward and recognition, organisational development, leadership, workforce development, workforce spend and workforce planning and employee culture, diversity and inclusion.
Membership and attendance
- Wendy Thomas (Chair), Non-Executive Director (4 of 5)
- Catherine Glickman, Non-Executive Director (4 of 5)
- George Lynn, Non-Executive Director (3 of 5)
- Kiran Mahil, Associate Non-Executive Director (1 of 5)
- Marika Stephenson, Director of People Services (4 of 5)
- Dr Hein Scheffer, Director of Strategy, Culture and Education (5 of 5)
Other members of staff are invited to attend as required.
The Board as Charity Trustee
The East of England Ambulance Service NHS Trust Charitable Funds Charity (The Charity) is registered with the Charities Commission for England and Wales (Registered charity number 1047987) and operates to raise funds to support the staff, volunteers, and local communities of the east of England, strengthening the provision of outstanding care to patients.
The Corporate Trustee is the sole Trustee, and it acts through the Board of Directors. Individual directors act as ‘agents’ of the Trustee and are not individual trustees. The Corporate Trustee is legally responsible for all the Charity’s activities.
Charitable Funds Committee
The Charitable Funds Committee was responsible for managing and monitoring the charitable funds held by the Trust on behalf of the Corporate Trustee. Membership and attendance
- Chris Brook (Chair), Non-Executive Director (4 of 5)
- George Lynn, Non-Executive Director (3 of 5)
- Omid Shiraji, Associate Non-Executive Director (1 of 1)
- Kevin Smith, Director of Finance (4 of 5)
Other members of staff are invited to attend as required.
Board Voting Directors
- Mrunal Sisodia: Trust Chair
- Wendy Thomas: Senior Independent Director. Chair, People Committee
- George Lynn: Non-Executive Director. Chair Audit Committee
- Catherine Glickman: Non-Executive Director. Chair, Quality Governance Committee. Chair, Remuneration and Nomination Committee.
- Chris Brook: Non-Executive Director. Chair, Charitable Funds Committee. Chair, Finance and Sustainability Committee.
- Julie Thallon: Non-Executive Director. Chair, Performance Committee
- Tom Abell: Chief Executive Officer (to 07 August 2024)
- Neill Moloney: Chief Executive Officer (from 2 September 2024)
- Kevin Smith: Director of Finance
- Marika Stephenson: Director of People Services (to 22 September 2024) Chief People Officer (from 23 September 2024) and Deputy Chief Executive (from 21 January 2025)
- Melissa Dowdeswell: Chief of Clinical Operations (to 21 March 2025)
- Simon Chase: Chief Paramedic and Director of Quality.
Non-voting Directors
- Simon Walsh: Medical Director
- Dr Hein Scheffer: Director of Strategy, Culture and Education 9to 31 October 2024). Director of Strategy and Transformation (from 1 November 2024)
- Kate Vaughton: Director of Integration and Deputy Chief Executive Officer ( to 1 September 2024)
- Jo Cripps: Interim Director of Corporate Affairs and Performance (to 27 September 2024)
- Kiran Mahil, Associate Non-Executive Director
- Victoria Corbishley, Associate Non-Executive Director
- Omid Shiraji, Associate Non- Executive Director
Declaration of Interest
The Trust is committed to transparency as such all members of the Board are required disclose any existing or potential interest that may be conflicted with their roles. As part of that commitment the Trust has published on its website an up-to-date register of interest, including gifts and hospitality for decision making staff within the past twelve months, as required by the ‘Managing Conflicts of Interest in the NHS’ guidance.
Annual Governance Statement
Scope of responsibility
As Accountable Officer, I have responsibility for maintaining a sound system of internal control that supports the achievement of the NHS trust’s policies, aims and objectives, whilst safeguarding the public funds and departmental assets for which I am personally responsible, in accordance with the responsibilities assigned to me. I am also responsible for ensuring that the NHS trust is administered prudently and economically and that resources are applied efficiently and effectively. I also acknowledge my responsibilities as set out in the NHS Trust Accountable Officer Memorandum.
The purpose of the system of internal control
The system of internal control is designed to manage risk to a reasonable level rather than to eliminate all risk of failure to achieve policies, aims and objectives; it can therefore only provide reasonable and not absolute assurance of effectiveness. The system of internal control is based on an ongoing process designed to identify and prioritise the risks to the achievement of the policies, aims and objectives of the East of England Ambulance Service NHS Trust, to evaluate the likelihood of those risks being realised and the impact should they be realised, and to manage them efficiently, effectively and economically. The system of internal control has been in place in the East of England Ambulance Service NHS Trust for the year ended 31 March 2025 and up to the date of approval of the annual report and accounts.
Capacity to handle risk
Risk management is recognised by the Trust as an integral part of good management practice, informing decision making and facilitating business planning process. The aim of risk management is to support the Trust’s vision and values by promoting a consistent and integrated approach across all parts of the organisation ensuring we are aware of our risks and are responsive not averse. All employees of the Trust must appreciate the importance of Risk Management, and their personal responsibility for the identification, prevention and control of risk.
Trust Board is responsible for providing strategic leadership to risk management throughout the Trust, including leading by example by adopting an open culture of risk awareness and continual learning. Trust Board is also responsible for ensuring robust internal controls are in place, which includes the provision of effective systems for managing risk, ratifying the risk policy and overseeing its effectiveness through receipt of sub-committee reports.
The Compliance and Risk Group provides assurance to the Audit Committee. The group foster an open, anticipatory, adaptive and proactive risk-aware culture in which people are actively engaged, ensuring risk is kept under prudent control on behalf of the Board and in accordance with the Board’s risk appetite, maintaining an effective control system and minimising over exposure to threats. The group also provides horizon scanning, check and challenge and keeping material risk under review and improving organisational resilience.
To improve and embed risk management culture and awareness staff are provided with training on the risk principles and management framework tools to support them in making informed decisions.
The risk and control framework
The Risk Management policy sets out the Trust’s approach to risk, acceptable appetite thresholds, roles/responsibility, monitoring and accountability arrangements on risk management.
The policy outlines principals on how we identify, evaluate, assess and monitor risks. The aim is to ensure that risk management is comprehensive covering all parts of the Organisation, recurrent not just one-off exercise but something that is maintained and kept up to date, integrated not just as an add-on but part of all operations and systems, suitable not a ‘one size fits all’ instead principles, policies and practices that can be adapted to any activity and being proportional maintaining a sense of perspective and proportion between benefits and risks.
Trust revised governance structures increased scrutiny and focus on risk oversight. The Audit Committee has the primary responsibility in providing assurance to the Board regarding effectiveness of the Trust’s system of integrated governance, risk management and internal control. Each of the Trust’s four Committees (Finance and Sustainability, Quality Governance, People, Performance and Compliance and Risk Group have responsibility for the oversight of specific risks associated to their respective remit.
Risk Leadership
The Trust Board has overall accountability for the effective and efficient management of the Trust and for ensuring the Trust adheres to the principles of good governance. The Chief Executive is accountable officer for the management of risk, responsible for maintaining sound internal control systems that supports achievement of the Board’s policies, objectives, whilst safeguarding funds and assets. Director of Governance supports the Chief Executive in the role as accounting officer of the Trust and has responsibility for risk in relation to corporate governance framework, compliance and assurance including the Board Assurance Framework.
Risk Management Training
Staff are trained and equipped to manage risk in a way appropriate to their authority and duties, in line with the Trust’s Risk Management Policy and complimenting guidance. The frequency and level of risk management training is identified through training needs assessments, ensuring that individual members of staff have the relevant training to equip them for their duties and level of responsibility.
Training staff is also embedded within the Corporate Induction, as well as annual refresher via e-learning mandatory training requirements. Quarterly training and support is given to management teams to help standardise approach to risk management. Risks registers are held on the Insight Risk System which allows for risk identification, management, and escalation in line with the Trust’s risk management policy. In addition, a range of complimentary policies to risk are in place and available to staff via the Trust’s intranet.
Risk is an important tool in identifying and managing learning across the Trust. Risk specialists attend governance groups to facilitate learning and horizon scanning for new and emerging risks, which is also informed by external reports including internal audit, NHSE and related regulatory recommendations.
Risk Management Strategy and Risk Appetite
The Board recognises that risk is inherent in the provision of healthcare, therefore has a defined approach in place to identify context ensuring that the Trust understands and is aware of risks it is prepared to accept in pursuing delivery of its objectives by providing clarity on acceptable levels of risk the Trust is willing and unwilling to take through defining its risk appetite. The Trust use risk appetite as a facilitating tool for decision making where there is uncertainty on outcomes in pursuit of value. Considered risks will be taken were for example, long term benefits out-weighs any short-term losses.
The Trust wide risk appetite statement is supported by individual directorates appetite statements outlining accepted tolerance thresholds levels and underpinning governance. This approach facilitates safe service planning, provide assurance to regulators and maximise opportunities through a balanced risk taking versus reward.
Quality Governance Arrangements
The Trust’s quality governance and leadership structure ensures that the quality and safety of care is being routinely monitored across all services. The development of this continues to embed to ensure that there is an underpinning role culture to support the delivery of an effective and efficient governance framework. The Trust has a robust set of quality governance arrangements in place, including:
- Committee and sub-group infrastructure to ensure all quality issues are monitored and addressed. This includes safeguarding, medicines management, health and safety and infection, prevention and control.
- A full suite of policies and procedures to control quality systems and processes.
- Robust quality impact assessment processes.
- Data quality checks within the processes for publishing and using performance information.
The Trust have a robust quality performance framework to streamline assurance flow through our committee structures. Risk management processes and reporting mechanisms are in place to review and challenge performance and variation. The Trust operate a culture of open and transparent reporting of incidents and risks.
Data Security Risks
The reporting and management of both data and security risks are supported by ensuring that all staff are reminded of their data security responsibilities through education and awareness. Data security training forms part of mandatory training requirements. Mandatory staff training is supported by a range of additional measures used to manage and mitigate information risks, including, physical security, data encryption, access controls, audit trail monitoring, departmental checklists and spot checks. The effectiveness of these measures is reported to the Information Governance Group and Finance Committee as well as the Trust’s SIRO. This includes details of any personal data-related Serious Incidents, the Trust’s annual Data Security and Protection Toolkit score and reports of other information governance incidents and audit reviews.
Significant Risks
Material risks in ability to operate efficiently, effectively and economically are outlined in the BAF which is reviewed at each of the Board sub-committees with assurance concerns escalated via Audit Committee to Board. The BAF provides a cohesive and comprehensive view of assurance across the risk environment. An opportunity to identify gaps in assurance needs that are vital to the organisation and addressing them. BAF risks are reviewed annually in alignment with any changes to revised risk appetite and strategic objectives.
In-year, the risks were reviewed, reassessed and strengthened with a summary as follows:
| Strategic Goal | Strategic Risk | Comments |
|---|---|---|
| 1: Be an exceptional place to work, volunteer and learn | SR1a: If we do not ensure our people are safe and their wellbeing prioritised, there is a risk we will be unable to attract, retain and keep our people safe and well | Staff burnout remains concerning across the Trust however, 2024/25 internal targets for Health and Wellbeing to support staff progressed well towards target, recruitment numbers are TRiM Practitioners at 188, Mental Health First Aiders at 173 and Wellbeing Champions at 276. Currently 787 people signed up to the Time for Me App and TRiM process under improvement review. |
| SR1b: If we do not ensure our leaders are developed and equipped, there is a risk that we will not be able to change our culture and value, support, develop and grow our people | The Trust published and implemented the inclusivity and governance plan which is monitored through People Committee. Leadership Development Programme has been successfully implemented with high attendance on core skills. However, bullying and harassment employment relations cases continue to fluctuate in line with employment relations case volume. | |
| 2: Providing outstanding quality of care and performance | SR2 If we do not deliver operational and clinical standards then there is a risk of poor patient outcomes and experience | C2 performance remain a concern, however, the trust has started to see some consistent positive improvements. This has been assisted by reduction in the average arrival to handover times. |
| 3: Be excellent collaborators and innovators as system partners | SR3 If we do not ensure we have the ability to plan, influence and deliver across our systems to secure change, we will not be able to meet the needs of our public and communities | Clinical strategy implementation plan and strong integration with system partners remain core components of East’s 2025/30 strategy approach. The risk has slightly reduced due to progress in Trust engagement with key partnership working groups across all ICBs |
| 4: Be an environmentally and financially sustainable organisation | SR4 If we do not resolve long standing organisational inefficiencies, we will be unable to deliver an effective, sustainable, value for money service to our public | Lessons learnt from 2024-25 business planning process have been incorporated and embedded into 25/26 process to improve culture of ownership of efficiencies and budget management. It is now highly likely that the Trust will achieve its financial plan for 2024-25. |
| All Goals | SR5 If we do not clearly define our strategic plans, we will not have the agility to deliver the suite of improvements needed | 2025/30 East strategy has been approved by the Board and supported by revised transformation governance arrangements to improve reporting and accountability through introduction of Portfolio and Programme Boards. |
| SR6 If we do not deliver sustainable regulatory compliance and develop positive relationships, we will have limited ability to deliver our strategy | Regulatory warning notices were issued against the Trust, interventions have been put in place to strengthen risk monitoring, oversight and accountability. Accountability Forums, Transformational Portfolio Board and Board sub-Committees continues to provide oversight support on regulatory compliance. |
Governance Compliance Risks
The Trust remain not fully compliant with the registration requirements of the Care Quality Commission. A range of mechanisms are in place to provide assurance of compliance with the Health and Social Care Act 2008 (Regulated Activities) and Regulations 2010, as set out in the Care Quality Commission’s guidance for providers.
The Trust had two warning notices associated with the s29a closed in 2024/25. There remain three open actions from the original s29a warning notice. The CQC issued a further warning notice in January 2025 and a section 64 warning notice for failing to meet requirements relating to staff training, staffing levels in Emergency Operation Centres, in adequate investigation of controlled drug incidents, call wait times, the culture of the service and acting on information from staff to develop and improve the service.
The Trust also received a notification of contravention from the Health and Safety Executive, concerns cited included the identification of risks and controls to prevent work related stress, in adequate systems to enable managers to support staff, staff awareness of policies and procedures, weaknesses in systems for monitoring and reviewing of work-related stress measures. The Trust continues implementing improvement plans which are monitored via the Rapid Quality Review Meeting.
Accountability forums and revised transformation governance through the formation of portfolio/programme boards with board sub-committee continue to provide oversight and assurance to board. Leadership workshops and training programmes on culture also continues to be implemented to support alignment with Trust values and behaviours across the Trust.
Well Led Framework
The Trust Board has continuously reviewed its effectiveness through a blended approach including not limited membership skills and experience competencies, a Board development plan bringing together opportunities for Board members to develop technical skills and knowledge as individual members and collectively as a board.
The Trust has seen improvement on culture, leadership development capacity and capability. The Trust had three equality diversity inclusive surveys each to understand the experiences of diverse staff, with feedback being provided to leadership teams via leadership briefing and communications.
The Trust reviewed and changed governance structure to reflect the changing needs of the organisation. This was further reviewed in Q3 2024/25, and small changes were made to ensure that the structure was effective and working as required. This structure has a clear mapping of metrics, risks, operational groups and transformation projects to board/committee. Board leadership has evolved with newly appointed Non-Executive Directors and the Chief Executive Officer to reflect the changing needs of the organisation especially in digital, logistics, organisational development and transformation areas.
External company, Guardian Service Ltd was appointed to deliver Freedom to Speak Up Service providing the organisation with a more comprehensive, independent and resilient service for 24/7 365 days the year.
Embedding of Risk Management
Risks are linked to our strategy and are reviewed as part of a dynamic use of our Corporate and Directorate Risk Registers. Risk management is embedded throughout key activities in the organisation, including:
- Transformation programmes
- Identification and assessment of risk is a core business function, with managers recognising and assessing risks to the delivery of their aspect of the service.
- All cost improvement programmes should have approved quality impact assessment, with mitigations where risks are identified.
- Embedded incident reporting system for staff to report incidents or near misses.
- Core groups monitor the risks relevant to their terms of reference.
- Audit Committee and Compliance Risk Group has oversight of risk management ensuring it is embedded
- All risk registers are managed via an electronic database. Escalation of risk is achieved through the governance structures and processes.
Workforce Strategies and Staffing Systems
Progress against the workforce plan is monitored through People Committee and Board. The service is committed to building an engaged and inclusive culture with engagement events for staff to speak directly with Executives and Non-Executive Directors, nominated Executive leads for each ICB area and ongoing joint working with Trade Unions to improve Workforce Policies and Procedures. The Trust is undertaking significant work to improve the culture and leadership in the organisation.
The Trust will continue to foster positive collaborative working relationships and ensure that existing staff networks (LGBT+, BME, Women, Men, Multi-Faith and Disability) are encouraged to play an active role in the decision making in the Trust.
Compliance with CQC Registration Requirements
The Trust remain not fully compliant with the registration requirements of the Care Quality Commission. The Trust was rated overall as requires improvement in July 2022 inspection. Two warning notices associated with the s29a warning notice were closed in 2024/25. There remain three open actions from the original s29a warning notice. The CQC issued a further warning notice in Jan 2025 and a section 64 warning notice for failing to meet requirements relating to staff training, staffing levels, in adequate investigation of controlled drug incidents, call wait times, the culture of the service and acting on information from staff to develop and improve the service.
The Trust also received a notification of contravention from the Health Safety Executive, concerns cited included identification of risks and in adequate controls to prevent work related stress, weak systems in place to enable managers to support staff, lack of awareness on policies and procedures, weaknesses in systems for monitoring and reviewing work-related stress measures.
The Trust continues implementing improvement plans which are monitored via the Rapid Quality Review Meeting.
The Trust undertook self-assessments against the Quality statements defined within the criteria of the CQC well-led review. The Trust Chair holds and maintains the ‘Fit and Proper Persons Test Register’ for the Board. Annual checks are carried out to ensure all those listed are fit and proper against the requirements defined by the Care Quality Commission. The Trust remain focused on making the necessary improvements, working with regulators to establish and deliver sustainable change.
Register of Interests
The Trust is committed to openness and transparency in its work and decision making. As part of that commitment the Trust has published on its website an up-to-date register of interest, including gifts and hospitality for decision making staff (as defined by the trust with reference to the guidance) within the past twelve months, as required by the ‘Managing Conflicts of Interest in the NHS’ guidance.
Pension Scheme
As an employer with staff entitled to membership of the NHS Pension Scheme, control measures are in place to ensure all employer obligations contained within the Scheme regulations are complied with. This includes ensuring that deductions from salary, employer’s contributions and payments into the Scheme are in accordance with the Scheme rules, and that member Pension Scheme records are accurately updated in accordance with the timescales detailed in the Regulations.
Control measures are in place to ensure that all the organisation’s obligations under equality, diversity and human rights legislation are complied with.
Equality, Diversity and Human Rights
Control measures are in place to ensure that all the organisation’s obligations under equality, diversity and human rights legislation are complied with. As part of the Trust’s culture improvement work, there is an inclusivity plan in place to deliver further improvements in relation to equality and diversity over coming years. The Trust has several inclusivity network groups across the Trust with budget allocations to promote their work and reporting to People Committee for assurance.
UK Climate Projections
The Trust has plans in place which take account of the ‘Delivering a Net Zero Health Service’ report under the Greener NHS programme. The trust ensures that its obligations under the Climate Change Act and the Adaptation Reporting requirements are complied with.
The Trust is undertaking several initiatives to ensure compliance including not limited, use of cleaner energy in its new hubs and electric vehicles. This is supported by a robust strategy and robust governance provide assurance and measure performance. During the year Trust Board had a development workshop to net-zero and sustainability to enhance understanding on their leadership obligations.
Review of economy, efficiency and effectiveness of the use of resources
The Trust’s Productivity and Efficiency approach relies on embedding a value for money culture within the organisation, through financial training and awareness, multi-professional working, an open and transparent approach around our challenges, advanced partnership working, using research, learning and best practice. The Trust has a range of processes to ensure that resources are used economically, efficiently, and effectively. This includes management and supervision arrangements for staff and a system of devolved budget management. This incorporates reviews of finance and performance at budget manager, service director and overall, Trust level, through detailed reporting to the Finance and Sustainability Committee. The Committee is supported by a number of sub-groups that provides assurance on the Trust’s efficiency and productivity programmes. Delivery reviews are supported by quality impact assessments.
External auditors are required as part of their annual audit to satisfy themselves the Trust has made proper arrangements for securing economy, efficiency, and effectiveness in its use of resources and report by exception if in their opinion the Trust has not.
Information Governance
In 2024-2025 there were a total of 30 cases reported to the Information Commissioner’s Office (ICO) through the data security reporting tool. Of these, at the time of writing this report, the ICO took no further action in all of the cases, being satisfied with the investigation and actions taken by the Trust. Any recommendations provided by the ICO are monitored at the Trust’s Information Governance Group and Audit Committee. An overview of the 30 incidents is as follows:
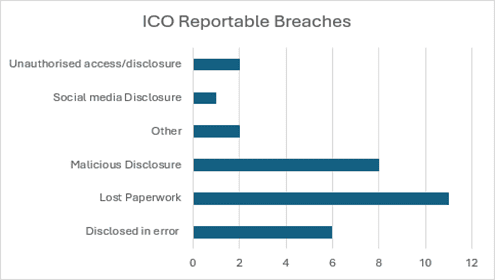
Following several incidents the Trust reported to the ICO, the ICO and the Trust agreed for a consensual audit to be carried out on the Trust’s data protection and freedom of information obligations. The audit consisted of a review on the following areas: Governance and Accountability, Subject Access Requests, Freedom of Information Requests and Organisational Awareness. EEAST were provided an assurance level of Reasonable across all areas, with an agreed action plan based on the ICO recommendations. This action plan is monitored at Information Governance Group.
Data quality and governance
The directors are required under the Health Act 2009 and National Health Service (Quality Accounts) Regulations 2010 (as amended) to prepare service Quality Accounts for each financial year.
This account looks back at performance in the last year and sets priorities for the following year. The Board approves the account prior to publication.
Arrangements are in place via trust wide groups to report quality and safety matters to the Quality Governance Committee, which in turn reports to the Board. This includes progress against the priorities set out in the Quality Account.
The Trust has processes in place to ensure that data is accurate and provides a balanced view. These include:
- Clinical data and outcomes checked and verified by the Clinical Audit Manager (State Registered Paramedic) prior to submission to the national audit programmes.
- Monthly checks of Department of Health statistical reports to ensure latest comparative data are included.
- Assurance through governance processes to Board-level via the Integrated Performance Report
- Data Security and Protection Toolkit
- Assurance provided through the Information Governance Group and the Data Quality and Security Group to Trust Board via the Audit Committee
- Regular scrutiny of processes and information through Board Sub-Committees
- Transition to the Data Lake – a single source of our data that cannot be manipulated.
Key risks to the data relate to the need for manual manipulation of aspects of the data set, due to multiple systems not yet interacting automatically with one another. Mitigations include the development of clear standard operating procedures for all data sets utilised. Operational data via the 999 and patient care records are assured as accurate as these are automated.
Review of effectiveness
As Accountable Officer, I have responsibility for reviewing the effectiveness of the system of internal control. My review of the effectiveness of the system of internal control is informed by the work of the internal auditors, clinical audit and the executive managers and clinical leads within the Trust who have responsibility for the development and maintenance of the internal control framework. I have drawn on the information provided in this annual report and other performance information available to me. My review is also informed by comments made by the external auditors in their management letter and other reports. I have been advised on the implications of the result of my review of the effectiveness of the system of internal control by the board, the Audit Committee and Quality Governance Committee and a plan to address weaknesses and ensure continuous improvement of the system is in place.
The Trust Board recognises the importance of the principles of good corporate governance and is committed to ensuring these are effective and efficient. This is implemented through key governance documents, policies, and procedures of the Trust, including:
- The Board Governance and Assurance Framework, including the Sub-Committees and groups.
- The Trust’s Standing Orders, Reservation of Powers to the Trust Board, Scheme of Delegation, Standing Financial Instructions and Trust Board Governance Assurance Framework
The Trust has a well-established expenditure control process. The requirement to use purchase orders for all applicable spend is also embedded. Both processes, together with the use of the authorised delegation limits and procurement requirements in the Trust’s Standing 12 Financial Instructions (SFIs), ensure that the Trust minimises unnecessary spend and ensures that value for money is considered before spending is incurred.
The Trust is led by a unitary Board, which provides leadership within a framework of internal control whilst promoting innovation, and challenge to performance issues. The Board monitors the effectiveness of the internal control systems and processes through clear accountability arrangements. Each Executive Director is held to account for control systems and processes, monitoring methods and weaknesses within directorates; cross checking evidence of compliance with statutory functions to ensure that the Trust remains legally compliant.
Review of Effectiveness of the Trust Board and Sub-Committees
The Trust reviewed its governance structures strengthening assurance oversight and scrutiny effectiveness. Board and Sub-Committees effectiveness are undertaken on annual basis. This also saw introduction of new Portfolio and Programme Board/s governance improving assurance effectiveness on change programmes and delivery of strategic objectives The Trust also undertook a skills and experience competence review to support development of board and committee members.
Summary of activities
The Board meets in public six times a year with a focus on patient voice and service user feedback, questions from the public, staff, student and volunteer voice. It also focuses on finance and performance reports and the Board Assurance Framework. Detailed reports have been received on a broad range of strategic and governance issues during the year.
To support the Board of Directors in fulfilling its duties effectively, Sub-Committees are formally established with Board approved terms of reference. The remit and terms of reference of these committees have been reviewed during the year to ensure continued robust governance and assurance. The importance of the triangulation of understanding, challenge and assurance between committees is recognised and reflected through cross-membership and reporting between committees and through the receipt of highlight reports to the Board of Directors.
The Board reviews its commitment to the codes of conduct and accountability for NHS Boards annually and is compliant with the codes of good practice for Boards, as applicable to a provider service NHS Trust of Corporate Governance Code. Committees in the corporate governance structure undertake an annual review of effectiveness ensuring that there are fit for purpose in the preceding year.
The Audit and Assurance Committee
The Audit Committee has non-executive director membership. It meets four times a year and reports to the Board annually on its work in support of the Annual Governance Statement. The primary roles of the committee are to independently monitor and review our internal control systems, risk management arrangements, and provide independent advice and assurance to our Trust Board.
Quality Governance Committee
The Quality and Safety Committee is chaired by a non-executive director, has two other non-executive director members and executive directors in attendance. It meets on quarterly basis for discussion and assurance that quality and safety arrangements are in place throughout the Trust and that they are working effectively. The committee has oversight of internal audits related to quality and safety. It also receives updates on any quality summits, and assurance from all key areas within its remit.
Clinical Audit activities
Clinical Audit forms part of the quality governance framework and provides assurance that services are being delivered to patients at the required standard, in order that the Trust meets the dimensions of quality: patient safety, patient experience and clinical effectiveness.
The results of audits and experience audits are used to review and develop training for staff, and examples, themes and trends have enabled the Trust to identify areas that draw out the quality measures.
The Clinical Audit and Patient Experience programmes for 2024/25 focused on national, strategic, and regulatory driven audit projects that related to the priorities set within the Quality Account agenda. Full details of all audits undertaken are in the Quality Account.
The Head of Internal Audit opinion and Annual Internal Audit Programme
17 internal audit reviews had been carried out with 7 receiving Reasonable Opinion, 3 Limited with 3 being Advisory and another 3 at Completion Stage at the time of writing the Annual Governance Statement. The Audit Committee has considered the outputs of this work when endorsing the 2024/25 AGS.
Head of Internal Audit’s Annual Opinion states: ‘TIAA is satisfied that, for the areas reviewed during the year, East of England Ambulance Trust has reasonable and effective risk management, control and governance processes in place.
This opinion is based solely on the matters that came to the attention of TIAA during the course of the internal audit reviews carried out during the year and is not an opinion on all elements of the risk management, control and governance processes or the ongoing financial viability or your ability to meet financial obligations which must be obtained by East of England Ambulance Trust from its various sources of assurance’.
Significant In-Year Matters
The Trust had an unannounced Care Quality Commission inspection in November 2024; no formal report has been issued yet. In January 2025 the Trust was issued with a Section 29A Warning Notice and a Section 64 (Regulation 17) under the Health and Social Care Act 2008, and below areas were recommended for improvement:
- The service did not ensure staff kept up to date with their mandatory training.
- Waiting times for calls were below national standards which meant the service did not ensure people could access the service when they needed it.
- The service did not have enough staff to keep service users safe from avoidable harm and or to provide the right care and treatment.
- The service had cultural issues across the three emergency operations centres sites and the emergency and urgent care sites.
- Not all controlled medicine incidents were properly investigated, appropriate action taken and recorded to mitigate further risks or lessons identified to improve future practice.
- Ambulance station areas did not all adequately act on information about staff opinion of the service to develop and take actions for improvement.
The Trust also received a notification of contravention from Health and Safety Executive on managing the causes of work-related stress, lack of systems in place to enable and encourage managers to support their staff, employees were unaware of policies and procedures, or experiencing difficulties in where to access information and weakness in systems for the monitoring and reviewing of work-related stress measures
Conclusion
I can confirm that there is no significant internal control issues identified that do not have a clear plan in place for effective mitigation. Where control issues have been identified, for example in relation to safe care and treatment and good governance through CQC inspection, a process has been developed which ensures appropriate support and scrutiny in relation to the areas required, with robust reporting in place. Improvement is being seen across all areas of concern.
There is an acknowledgement that the Trust continues its improvement journey, with strengthened systems and controls being implemented to mitigate the internal control challenges that the Trust is actively managing. I am confident that appropriate mitigation plans are in place with clear oversight and scrutiny through the regulators and that we therefore have a generally sound system of internal control that supports the achievement of our policies, aims and objectives. We continue to identify opportunities to strengthen the internal control environment into 2025-26.
Neill Moloney, Chief Executive Officer - June 2025
