Annual Quality Account 2024-2025
Date published: 25 June 2025
Summary
Welcome to the East of England Ambulance Service NHS Trust Quality Account for 2024/25. This document has been approved by the Trust Board and is an accurate account of the level of quality of service provided to patients. In developing this Quality Account, we have set out a summary of achievements for 2024/25 and goals for 2025/26 as mandated within the regulatory guidance.
In this report
- Part One
- Foreword and statement on quality from the Board
- Welcome to the East of England Service NHS Trust (EEAST) Quality Account
- Introducing the East of England Ambulance Service NHS Trust Quality Account and Improvements
- What is a Quality Account and what does it mean to EEAST and the people we serve?
- Our current quality position
- Care Quality Commission
- Department of Health Core Quality Indicators
- NHS Number and General Medical Practice code validity
- NHS clinical coding error rate
- Data quality
- Data security protection toolkit
- Statement of Accountability
- Part Two:
- Quality improvement initiatives
- Priority one: Patient safety
- Priority Two - Clinical effectiveness
- Priority Three - Patient Experience
- Part Three
- Progress on the quality account priorities 2024/25
- Performance of the Trust against quality metrics
- Achievements against local priorities set for 2024/25
- Clinical audit
- Participation in research
- Patient Safety Incidents
- Serious Incidents
- When things go wrong
- Duty of Candour
- National Patient Safety Alerts
- Patient experience and feedback
- Patient and public involvement
- Raising concerns and Freedom to Speak Up
- Working with our local communities
- Commissioning for Quality and Innovation (CQuIN)
- Quality success throughout the year
- Quality Governance Committee Assurance
- Statements from stakeholders
- Glossary
Part One
- Foreword and statement on quality from the Board
- Welcome to the East of England Service NHS Trust (EEAST) quality account
- Introducing the East of England Service NHS Trust (EEAST) quality account and Improvements
- What is a quality account and what does it mean to EEAST and the public we serve
- Our current quality position
- Care Quality Commission
- Department of Health quality indicators
- NHS number and General Medical Practice Code validity
- Clinical coding error rate
- Data Quality
- Data Security Protection Toolkit
- Statement of accountability: Chief Executive Officer, Neill Moloney
Foreword and statement on quality from the Board
At the East of England Ambulance Service NHS Trust (EEAST) our unwavering commitment to patient care and staff wellbeing drives every aspect of our operation. We strive to deliver an outstanding service whenever and wherever our patients need it, and to enable and empower our people to work in an organisation which is inclusive, responsive to their wellbeing needs and fosters a culture of excellence. Reflecting on the last year, we recognise the challenges we have faced, and the improvements delivered with the support of our staff, communities and regulators.
We continue to work to reduce our C2 response times to ensure our patients receive the right care, at the right time. We have implemented a range of strategies to support this such as increasing our collaboration with community providers to support patients to access alternative sources of care where clinically appropriate. For example, the unscheduled care co-ordination hub in Norfolk and Waveney has diverted 62% of their calls from the stack since its launch in September 2023, avoiding unnecessary ambulances responses while improving patient outcomes and system efficiency. In 2024, a total of 46,864 calls were passed via our Access to the Stack process across the Trust.
The single biggest contributor to C2 response times is hospital handover delays. In November 2024 the Trust launched handover 45 with the support of commissioners and acute Trusts. The primary aim is to reduce avoidable harm, in communities as a result of delayed ambulance response times, which are consequential to delayed handovers of emergency patients at acute trusts. Where handover of patients from the ambulance service to hospitals in 45 minutes has been delivered consistently, avoidable harm has demonstrably reduced.
The Trust continues to deliver on its cultural change journey to support and improve the wellbeing of our people. In the last year, we have restructured our operational directorate to ensure the spans of control for any single manager have reduced to a level which enables them to meet the needs and support requirements of the staff they are responsible for.
We have also launched a new 24 hour, 365 day a year Freedom to Speak Up Service to enable our staff to feel confident to speak up and raise their concerns in a safe, independent, resilient and confidential space. We have enhanced our wellbeing offering with the launch of the time for me app to support our staff to pro-actively manage both their mental and physical health and we have also implemented wellbeing rooms across the Trust. These changes are just one step in ensuring our people are working in an organisation in which they feel supported and empowered by an organisation which listens to their concerns and takes action based on their feedback.
We have taken a number of actions to ensure we continue to deliver a quality service for our patients and communities including:
- CQC: We have now delivered over 94% of the outstanding actions from the 2022 CQC inspection.
- Staff survey: A range of indicators showed an improvement in the last NHS Staff Survey, with more staff reporting that they felt they could report experiences of harassment, bullying or abuse following the speak out campaign, staff reporting they had not experienced discrimination from patients and service users and more staff reported there were enough staff to do their job properly which improved following a drive in recruitment across clinical operations. We recognise there is more to do, but as a Trust we are committed to maintaining this journey to excellence.
- Bury St Edmunds Ambulance Hub: The Trust officially opened its first net zero ambulance hub in Bury St Edmunds. This hub not only supports the Trusts carbon ambition but also maximises ambulance time on the road through the on-site vehicle repair workshop and supports staff wellbeing with the inclusion of a quiet room, multi-faith room, nursing room, gym and outside wellbeing space for rest and relaxation.
- Leadership Development Framework: The Trust continues to implement the leadership development framework for all senior leaders to empower them with the skills and knowledge to support positive change and improvement.
- Collaboration: The Trust launched urgent and emergency care hubs in all counties in partnership with the ICB’s to ensure patients are receiving the right care, first time, avoiding hospital admissions.
As we move into the next year, our commitment to enhancing patient outcomes and fostering a culture of excellence remains steadfast. These improvements would not be possible without the support of our people, volunteers, partners and communities. We are committed to maintaining the highest standards of care for our communities as an organisation which acts with unwavering integrity, and a workforce which is accountable, respectful, and strives to be excellent.
Neill Moloney
Chief Executive Officer
Welcome to the East of England Service NHS Trust (EEAST) Quality Account
Welcome to the East of England Ambulance Service NHS Trust Quality Account for 2023/24. This document has been approved by the Trust Board and is an accurate account of the level of quality of service provided to patients. In developing this Quality Account, we have set out a summary of achievements for 2023/24 and goals for 2024/25 as mandated within the regulatory guidance.
Improving quality is an overarching priority of the Trust and this report lays out plans for developing future services to improve the quality and safety of patient care and patient outcomes.
In order to help do this, the Quality Account is based on data from a range of sources.
Further information about us and our achievements can be found in our Annual Report.
Assurance for quality and safety is given to the Trust Board by the Quality Governance Committee which is in turn informed by our Compliance and Risk Group.
Underpinning the Compliance and Risk Group are a number of groups which cover the multiple aspects of our service including; risk management, patient safety, medicines management, safeguarding, infection prevention and control, medical devices and patient experience.
Information on all groups and how other factors contribute to this such as Healthwatch, internal audit and regulatory inspections can be further in the report.
Contributions to this document
All Integrated Care Boards (ICB) including Ipswich and East Suffolk ICB (the lead commissioner), HealthWatch groups and the region’s health overview and scrutiny committees (HOSCs) have been invited to provide a commentary on the provision of our quality and care to include within this document. Those received can be found in the Statements from Stakeholders section towards the end of this page.
Where can you get hold of this document?
This Quality Account is available on our website or write to: East of England Ambulance Service NHS Trust Headquarters, Whiting Way, Melbourn, Cambridgeshire, SG8 6EN.
If you require this document in another format or language, please contact our Patient Advice Liaison Service (PALS) on 0800 028 3382 or by emailing feedback@eastamb.nhs.uk.
Other sources of information
We publish a number of other documents which you may find useful, these include; Trust Annual Report, Safeguarding Annual Report and the Infection Prevention and Control Annual Report. These, and other information about us, can also be found on our website.
Introducing the East of England Ambulance Service NHS Trust Quality Account and Improvements
Our Trust provides urgent and emergency care services throughout Bedfordshire, Cambridgeshire, Essex, Hertfordshire, Norfolk and Suffolk.
During 2024/25 we also provided non-emergency patient transport services for patients needing non-emergency transport to and from hospital, treatment centres and other similar facilities within parts of Essex, Bedfordshire and Hertfordshire.
We work with six Integrated Care Systems (ICS) covering an area of approximately 7,500 square miles with a resident population of around 6.3 million people.
We employ more than 5,000 staff operating from over 100 sites and are supported by more than 1,000 dedicated volunteers working in a variety of roles including: Community first responders; volunteer car drivers; BASICS doctors; chaplains and our community engagement group.
The Trust Headquarters is in Melbourn, Cambridgeshire and there are ambulance emergency operations centres (EOC) at each of the three locality offices in Bedford, Chelmsford.
The east of England is made up of both urban and rural areas with a diverse population. As well as a resident population of about 6.3 million people, several thousand more tourists enjoy visiting our area in peak seasons each year. Our area also contains several airports including London-Luton and London-Stansted as well as major transport routes which increase the number of people in our region on a daily basis.
We have four areas of service provision:
Response to 999 calls as an emergency and urgent care service
In 2024/25, our emergency operations centre (EOC) received 1,472,933 emergency contacts from the public. On average, over 2,950 emergency 999 calls came into the ambulance service every day.
Call handlers record information about the nature of the patient’s illness or injury using sophisticated software to make sure they get the right kind of medical help. This is known as triaging and allows us to ensure that the most seriously ill patients can be prioritised and get the fastest and most appropriate response.
More information on how we manage these calls can be found within the Response Times section (page 23) of this report.
Special and partnership operations
The Trust operates two hazardous area response teams (HART) and has a resilience and emergency planning department who work closely with critical care charities and community volunteers to respond to a variety of emergency situations.
Scheduled Care Service – Patient Transport Service
We operate a quality Non-Emergency Patient Transport Service (NEPTS), working in collaboration with hospitals and treatment centres, transporting and caring for a variety of patients, including elderly and vulnerable people and those with mental ill health, to and from outpatient clinics, day-care centres and other treatment facilities.
Staff are trained to lift and manoeuvre patients in and out of vehicles, ensuring patients are safe and comfortable during the journey and arrive on time for appointments. Staff are also trained to administer first aid or life saving techniques should this be necessary. Other duties include making sure vehicles are clean and tidy, in line with infection and prevention guidelines and keeping accurate records of journeys. During 2024/25 we undertook 365,166 patient journeys and 36,719 escort journeys – a total of 401,885 NEPTS journeys.
Commercial services
We operate a number of commercial services that generate income for the trust, as well as providing organisational resilience.
CallEEAST, our non-emergency and commercial contact centre, offers an array of contact centre solutions to commercial organisations and NHS Trusts. The team supports 80 separate contracts handling in excess of 850,000 calls every year.
The National Performance Advisory Group (NPAG) brings people together nationally to share best practice and showcase industry developments across the NHS enabling innovation and efficiency.
TrainEEAST, the Trust’s commercial training department offers a wide range of first aid and emergency care training courses for businesses, organisations, individuals and our own people.
What is a Quality Account and what does it mean to EEAST and the people we serve?
A Quality Account is a mandatory report about the quality of services an NHS healthcare trust provides and is required to be completed in line with the Health and Social Care Act 2012.
Quality reports and accounts are set against the framework of three overlapping key themes, patient safety, clinical effectiveness and patient experience, which can be used to define quality of care.
The content is defined by NHS England and includes outcome results against specific indicators under five headings:
- Preventing people from dying prematurely.
- Enhancing quality of life for people with long term conditions.
- Helping people to recover from episodes of ill health or following injury.
- Ensuring that people have a positive experience of care.
- Treating and caring for people in a safe environment and protecting them from avoidable harm.
In addition to information provided within this report, our newly published Corporate Strategy 2025/30 details what we are aiming to achieve over the next five years and how we are going to do this.
Our current quality position
In my second quality statement, I remain proud that over the past 12 months, despite the increases in demands for the ambulance service, the Trust has continued to maintain its ambulance care quality indicators and has improved its ambulance responses in category 2, 3 and 4 calls. We have continued to work closely with the healthcare systems with increasing advance practice in urgent care along the expansion of Unscheduled Care Hubs across all areas of the Trust and successfully introduced artificial intelligence within our Emergency Operational Centres.
All members of the Board and I remain committed to drive and focus on quality and safety with the aim of improving pre-hospital clinical outcomes and the overall experience of our patients.
At the time of writing this statement the Trust has received a Section 64 notification from the (Care Quality Commission) CQC that requests further improvements to be made particularly to Category 2 responses. Several initiatives have been introduced over the previous year to help further improve all responses and include the implementation of a system lead initiative by the Trust in facilitating quicker hospital handovers, to further collaboration with other healthcare partners, to ensure alternative care pathways are available when required. Furthermore, improving the clinical workforce with a blend of Advanced Paramedics and Practitioners to help supervise and build confidence in staff decision making will aim to support a further drive in efficiency.
I can report that the Trust has been inspected in November surrounding its Urgent and Emergency Care function that led to a s29a Warning notice by the CQC, which requires the Trust to focus on improving mandated training compliance, medicine management investigations, call pick up performance and looking to engage better with the staff and continue to work on the cultural improvements recognised in the CQC feedback.
Whilst disappointing to receive the notification from the CQC, the Trust and I accept and remain committed to deliver a quality service to the community within the east of England and it is pleasing to report that all mandated training is now above the required target of 85% for all staff groups and competencies.
Following the on-site inspection in November, the Trust has been working to improve on the areas raised with oversight from our lead commissioners, the CQC and NHSE. Furthermore, I am pleased to update that progress has been made since the last report published in 2022, when the Trust was rated as ‘Requires Improvement’. The Trust continues to work hard with all system partners and regulators to ensure all our required actions are met and over 95% of the must dos and should dos from the 2022 report have been closed – an overview of our CQC progress can be found on page 11 of this report.
During 24/25 the Trust completed its largest ever staff and stakeholder collaboration approach that has led to reshaping the clinical strategic vision and the introduction of our new values and behaviours framework. To build on this, the Trust is launching a second staff wide stakeholder engagement event in 25/26 to help understand how we can bring those positive behaviours to life and make this an organisation that the staff would recommend and feel safe and able to be the true version of themselves. On the back of the success the Trust had with Clever Together, they have been recommissioned to assist in promoting the quality improvements required to make the Trust a great place to work through the ‘BIG conversation’.
Reviewing performance against the priorities for 2024/25, it is great to see how much progress has continued from the year before. Clinical supervision continues to grow and continued learning from complaints, clinical incidents, patient, staff, and community experiences helps provide constructive feedback to continue to develop our services for the better. One area that has really assisted staff is through the After-Action Reviews. The Safety team are aiming to deliver training to all clinical managers over the next year, which will help embedding learning from events where the Trust aim to concentrate on better decision making at scene; that will enable a more efficient workforce to respond quicker to patients waiting and build confidence in safer discharge to alternative pathways. These are areas that start to shift the care into the community with the aim to free up resources to those patients who are in an emergency. And for the fifth year running, we have exceeded the national ambulance average for our quality indicators; heart attack, stroke, and cardiac arrest survival to discharge for those patients where the arrest was bystander witnessed, and the initial heart rhythm was ventricular fibrillation or ventricular tachycardia (Utstein comparator).
Therefore, in summary the Trust has strived to continue to make improvements within the quality and safety portfolio as well as our operational performance and accept the feedback from the CQC that further improvements are still required. Neither I nor the Board do not underestimate the work we have ahead of us to ensure sustainable improvement.
The focus remains on improving a timely response to our communities whilst supporting an inclusive and safe culture that will lead to providing the best clinical care and develop further partnerships to deliver the best and required healthcare as an ambulance service of the future.
Simon Chase
Chief Paramedic (Allied Health Professional) & Director of Quality
Care Quality Commission
The Care Quality Commission (CQC), England’s independent regulator of health and social care ensures fundamental standards of quality and safety are met and sets out what good and outstanding care looks like. Then, through inspections, ratings and published reports, it encourages care services to meet those standards. The CQC inspect organisations through the five Key Questions using the CQC Single Assessment framework to determine whether:
- we are safe.
- we are effective.
- we are caring.
- we are responsive to people’s needs.
- we are well led.
Following a CQC inspection undertaken in 2022 where the Trust received an overall rating of ‘Requires Improvement’, an action plan was developed to take in to account the areas of improvement required as identified by the CQC; provision of mandatory training and appraisals to all appropriate staff, adequate staffing levels, continued development of staff engagement processes, response times and facilities/premises improvements.
67 deliverable actions were identified, and together with two long term actions from the previous plan, work began on completion.
To date, 65/69 (94.2%) have been closed with the remaining actions being those contained within our much longer-term priorities regarding, C2 response times, workforce development and the Trust’s cultural journey.
On 19 November 2024, the CQC commenced their onsite (unannounced) inspection of Urgent and Emergency Care (UEC) and our Emergency Operations Centres (EOC), visiting all three EOC sites and several ambulance stations throughout the region. This was followed with focus groups held with our EOC staff in January 2025. At the time of writing this report, the Trust is awaiting receipt of the draft inspection report from the CQC. In addition, we anticipate a ‘Well-Led’ assessment from CQC soon.
Unfortunately, some of the areas highlighted in the 2022 inspection report were again found to be a cause of concern for the CQC. On 23 January 2025, the Trust received a Section 29A Warning Notice relating to;
- Completion of mandatory training.
- Waiting times for calls
- Insufficient staff within EOC provision
- Culture of the organisation
- Investigation of medicines incidents
- Not acting adequately on information about staff opinion of the service to develop and take actions for improvement.
In addition, on 27 January 2025, the CQC served a Section 64 letter which detailed some of their findings from the recent assessment. This included a breach of Regulation 17 (Health and Social Care Act 2008 (Regulated Activities) Regulations 2014: Regulation 17 (Good Governance)) and Regulation 12 (Health and Social Care Act 2008 (Regulated Activities) Regulations 2014: Regulation 12 (Safe care and treatment)).
In line with NHS guidance, the Trust is required to participate in a Rapid Quality Review (RQR) meeting, the membership group of which includes EEAST representatives, Suffolk and North East Essex Integrated Care Board (ICB) (lead commissioner, NHS England and the Care Quality Commission).
A set of metrics were developed to take in to account the CQC’s findings and the Trust’s ambition to drive improvement and close identified gaps, which have been presented at two RQR meetings to date. At the time of this report, the Trust has exceeded the set trajectory for statutory and mandatory training and is meeting the trajectories for other metrics relating to the investigation of medicines incidents, staffing within EOC and call pick-up time. Metrics relating to culture and acting upon staff feedback are in development stage as part of the identified improvement plan for each area.
The following provides information on actions taken or planned and improvements seen since January 2025.
Statutory/Mandatory training
A review was undertaken by the Learning and Development team to ensure that the Trust’s statutory/mandatory topics were consistent with the eleven defined within the national Core Skills Training Framework (CSTF).
Once completed, staff were informed of the topics that should be completed as a minimum and the expectation for them to be completed.
The Trust also provided additional level three safeguarding training sessions.
At the end of January 2025, the Trust was achieving an overall level of 83.0% compliance with the CSTF topics, this steadily improved over the following weeks and at the end of March 2025, reached 92.6% compliance. This will continue to be monitored during 2025/26 to ensure compliance does not reduce below the 85% level expected by the CQC.
Staffing within our Emergency Operations Centre
The table below shows our target for call handlers, dispatchers and clinical assessment service staff and our staffing levels as at 24 March 2025 for each of these groups.
| Staff group – workforce effective (employed and agency) | Target | 24 March 2025 | Within recruitment pipeline |
|---|---|---|---|
| Call handlers | 255 | 251 | 17 |
| Dispatchers | 123 | 118 | 8 |
| Call pick-up 95th centile | 128 | 99 | 32 |
Call pick-up times
For these key performance indicators, the Trust, like all other ambulance services, reports against two measures for answering 999 calls within 5 seconds; the mean and the 95th centile.
For the year 2024/25, we achieved a mean of 12 seconds and a 95th centile of 1 minute and 25 seconds.
For the year 2025/26, we are currently achieving 2 seconds for the mean and 1 second for the 95th centile (as at 8 May 2025).
Medicines management
Following the concerns raised by the CQC regarding the management of medicine investigations, a number of actions were taken including a weekly review by the Trust Pharmacist and Deputy Clinical Director of all reported incidents to ensure that no medicines incidents were closed without any lessons learned being recorded. Since the 01 February, this has been achieved with learning shared with operational teams. This will continue to be monitored with oversight undertaken by the Medicines Management Group who report to our Compliance and Risk Group.
Culture
A number of actions have already been taken since the inspection in November 2024;
- Publication of NHS staff survey (2024) results which demonstrate that EEAST was the most improved ambulance service for the third year running
- Launch of the new Trust values
- Launch of ‘Big Conversation’ on what matters most for all staff, with dedicated physical and virtual session for EOC
- Launch of health and wellbeing passport
- Implementation of sexual safety training.
Whilst some improvements have been seen, we acknowledge that there is further work to be done and outcomes from the ‘Big Conversation’ events will help shape future actions.
Staff engagement
The final concern raised by the CQC within the Section 29A warning notice, was that we were not acting adequately on information about staff opinion of the service to develop and take actions for improvement.
As for the culture plan, the ‘Big Conversation’ events will help with this piece of work and monitoring of defined key performance indicators will be undertaken through our accountability forums.
On 17 April 2025, a decision was made by the RQR group membership, that due to the sustained changes achieved since February, the Trust could move to the exit criteria stage.
From a previous inspection in 2020, the Trust was also given notice under Section 31 of the Health and Social Care Act with seven conditions relating to; safeguarding, staff allegations, recruitment checks, Disclosure and Barring Service (DBS), contracted private ambulance service provision, sexual harassment and processes to manage concerns, grievances and disciplinaries. To date four of these conditions have been lifted; Safeguarding, staff allegations, recruitment checks, Disclosure and Barring Service (DBS) checks.
At the time of this report, we are awaiting the outcome of the remaining three; contracted private ambulance service provision, sexual harassment and processes to manage concerns, grievances and disciplinaries, which the CQC have advised are being considered alongside the latest inspection report.
Next steps
Work will continue embedding the actions already implemented and closure of those still ongoing as well as continuing to sustain the improvements seen in response to the Section 29A Warning Notice and Regulation 64 letter.
As agreed within the RQR process, metrics, supported by narrative summaries, will be monitored through our commissioner led regional quality and safeguarding group.
In support of the cultural work, we will be asking our ICB colleagues to undertake a quality engagement visit within their respective areas, we are hoping that these will be completed by the end of September 2025.
We are anticipating recommendations being included within the November 2024 CQC inspection report which will inevitably result in a new improvement plan and there is also a possibility that the Trust will be assessed at an overall Trust wide level for the key question of Well-Led in spring 2025.
Our Quality Statements will be reviewed at six-monthly intervals to provide assurance regarding compliance to identify any emerging gaps. Although already available to our staff, these will be published on our Trust website within the year, however this is dependent on any further changes that the CQC implement.
| Overall trust quality rating | |
|---|---|
| Are services safe? | Requires improvement |
| Are services effective? | Requires improvement |
| Are services caring? | Good |
| Are services responsive? | Requires improvement |
| Are services well-led? | Requires improvement |
Department of Health Core Quality Indicators
All NHS organisations are required to report against a set of Core Quality Indicators (CQIs) relevant to their type of organisation. For ambulance trusts, both performance and clinical indicators are set as well as indicators relating to patient safety and experience.
Where information is publicly available, organisations are also required to demonstrate their performance against other ambulance services within the year.
| Ambulance response times (categories 1-4) | |||
|---|---|---|---|
| C1 | Immediately life-threatening injuries and illnesses | 7 minutes mean response time | 15 minutes 90th centile response time |
| C1T | Immediately life-threatening injuries and illnesses where the patient is transported to hospital | 7 minutes mean response time | 15 minutes 90th centile response time |
| C2 | Emergency | 18 minutes mean response time | 40 minutes 90th centile response time |
| C3 | Urgent calls and in some instances where patients may be treated in situ (e.g., their own home) or referred to a different pathway of care | 120 minutes 90th centile response time | 120 minutes 90th centile response time |
| C4 | Less urgent. In some instances, patients may be given advice over the phone or referred to another service such as a GP or pharmacist | 180 minutes 90th centile response time |
.
| AMBULANCE CLINICAL OUTCOMES: ACUTE ST-ELEVATION MYOCARDIAL INFARCTION (STEMI). Patients who undergo a pre-hospital assessment for STEMI (heart attack), diagnosed at the earliest opportunity and given specifically tailored care. |
|---|
| The percentage of patients with a pre-existing diagnosis of suspected ST elevation myocardial infarction who received an appropriate care bundle from the Trust during the reporting period. |
| An appropriate care bundle is a package of clinical interventions such as oxygen therapy and the giving of relevant drugs that are known to benefit patients’ clinical outcomes. |
| Previously ambulance trusts were also required to report on the stroke diagnostic bundle, however this was removed from the national programme in 2023. |
NHS Number and General Medical Practice code validity
Ambulance trusts are excluded from this requirement therefore no records were submitted during 2024/25 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics.
NHS clinical coding error rate
As an ambulance service, EEAST was not subject to the Payment by Results clinical coding audit during 2024/25 by the Audit Commission.
Data quality
The digital services organisation within the Trust provides technology to support the operational activities and corporate service areas, digital transformation technology programmes, information repositories and data services. NHS England benchmarked all English trusts in the year (the Digital Maturity Assessment) and EEAST were in the top quartile in the ambulance services category and at the national average for all trusts.
The Trust Electronic Record Platform has now achieved the benchmark of over 96% digital utilisation for all patient interactions which the Trust will target to get to 100% in the years to come, the Trust mobile clinicians also have access to the National Care Records Service to enable access to longitudinal records.
The core clinical platforms maintained very high availability in 2024/25, with no major disruption. The organisation’s digital services through the year maintained the continued service to the wider Trust staff with a continued reduction in time to resolution despite a significant increase in the demand for new services. During the year, further new technology has been deployed in support of national guidelines to further protect the organisation against the continual cyber challenges, this work never ends, and we will continue this into the coming years.
The digital services team continued to deliver the Trust’s published Digital Strategy with a move from physical environments to virtualised external data centres and cloud-based technology in line with NHS best practice. The strategy was reviewed and has been adjusted to support the core Trust strategies.
As a Trust we receive over two and quarter million emails per month and send an average of three hundred and sixty thousand emails every month internally and externally. The Trust has over seven thousand end user devices all with connection to the internet. Through the year, whilst we saw daily unauthorised attempts to access our systems including multiple brute force attacks, the integrity of all our digital systems and assets were protected and maintained.
The Trust has several processes in place to ensure that data included within the Quality Account is accurate and provides a balanced view. These include:
Clinical data and outcomes
- checked and verified by the clinical audit manager prior to submission to the national audit programmes,
- monthly checks of the department of health statistical reports to ensure latest comparative data is included,
- digital data quality checks are automated with tooling with exceptions identified for the resolving process, -assurance through internal governance processes to board level via the integrated board report.
Data Security Protection Toolkit
- Assurance provided through Information Governance Group to Trust Board via the Audit Committee.
- Regular internal and external scrutiny of processes and information through a number of groups and committees.
Data security protection toolkit
For the 2024/25 assessment, the Data Security Protection Toolkit (DSPT) has adopted the National Cyber Security Centre’s Cyber Assessment Framework (CAF) as its basis for cyber security and information governance assurance, moving away from the ten Data Standards which have been used since 2018. The Trust, along with other larger NHS organisations, have been moved to the CAF aligned DSPT. The DSPT also provides the Trust with a means of reporting data breaches and data security incidents.
The CAF Aligned DSPT is split into objectives, principles and outcomes covering the following areas: Objective A managing risk, Objective B protecting against cyber-attack and data breaches, Objective C detecting cyber security events, Objective D minimising the impact of incidents, Objective E using and sharing information appropriately.
EEAST are required to assess against 47 outcomes across the five objectives, each outcome is assessed against a set of statements that fall into categories of “not achieved”, “partially achieved” or “achieved”. NHSE have determined the expected achievement level for each outcome to enable an organisation to meet standards met. NHSE have stated it has not been designed to reach “achieved” on all outcomes. Twelve of the outcomes have an increase in requirements to achieve standards met and there are six outcomes where organisations can assess themselves as “not achieved” this year, however it is expected these will increase in future years.
This year’s baseline submission was moved forward to 31 December 2024, with the final submission for the assessment being 30 June 2025.
At the time of this report, the status of the CAF aligned DSPT is that of the 47 outcomes:
- 34 meet the expected outcome required
- 13 do not meet the expected outcome required, however three outcomes of these match NHS England’s result of ‘not achieved’.
Each Outcome requires a statement explaining how the Trust has achieved each outcome and to supply evidence to support the statement.
The information governance team hold frequent meetings with the Trust’s digital team to concentrate on those areas which have not met the expected level, to identify whether the Trust can achieve the outcome, or if there is a requirement of work to be undertaken before June 2025 and the final submission.
Progress against these outstanding areas will be monitored through our Information Governance Group and assurance provided to the Trust Board through our Audit Committee.
Statement of Accountability
As Accountable Officer and Chief Executive of the Trust, I have responsibility for maintaining the performance and standards achieved within our services, and to support an environment of continuous quality improvement.
This Quality Account has been produced by the East of England Ambulance Service NHS Trust, in line with the requirements of the Health and Social Care Act 2012. The Quality Account contains details mandated by the regulations alongside the measures that the Trust, in association with our NHS and public partners, has decided will best demonstrate the work that has been done to maintain and improve the standard and quality of care we provide to our communities.
This account sets out the work has been undertaken this year to improve the quality of care to patients and outlines where we want to improve to ensure all patients have a positive experience and the standard of care that we want.
As accountable officer, it is also my responsibility to ensure both the quality and accuracy of the data within this Quality Account and to confirm that it presents a balanced picture of the Trust’s performance. Therefore, to the best of my knowledge the information contained within this Quality Account for the East of England Ambulance Service NHS Trust is a true and accurate record.
Neill Moloney Chief Executive Officer
Part Two:
- How have we prioritised our quality improvement initiatives
- Priority One - Patient safety
- Priority Two - Clinical effectiveness
- Priority Three - Patient experience
Quality improvement initiatives
The Quality Account for 2025/26 will continue to focus on the core priorities which match the mandatory indicators for ambulance trusts set by the Department of Health and Social Care (DHSC) as outlined in Part 1 as well as local priorities to improve the quality of care delivered by our staff.
The National Quality Board (NQB) has currently paused its review of the required content for quality accounts, so this report has been compiled in line with current published guidance.
The following tables provide information on the chosen priorities under the three headings of;
- patient safety
- clinical effectiveness, and
- patient experience.
As well as the reason for choosing them and what we hope to achieve over the next 12 months.
Priority one: Patient safety
| Priority | Why we have chosen this priority | What we are trying to improve | What success will look like |
|---|---|---|---|
| To further embed the Learning from Deaths (LfD) process at EEAST. | To improve the processes around data collection and structured judgement reviews which in turn will allow for themes of improvement and excellence to be clearly identified. This will lead to improvements in care, overall patient safety as well as maximise learning. | Automate the reporting processes for LfD by integrating incident reports onto a dedicated mortality module on the Datix system. Create feedback pathways to staff to allow excellence and improvement themes to be easily shared | A functional and fully automated mortality module to streamline the LfD process and effectively record data. Staff gaining feedback on LfD reviews in a timely manner to maximise learning across the organisation (reporting of number and timeframe for feedback). |
| Enhance the way in which we share learning from incidents, complaints and claims. | Sharing of learning identified as part of a review process is pivotal to drive a positive safety culture and improve safety for staff and patients. | Make learning accessible to all staff via multiple platforms rather than reliance on safety alerts and monthly newsletters. Utilise Trust devices and applications to share identified learning i.e. Class Publishing, JRCALC APPs. | Multiple ways for teams to share learning easily across the organisation. System learning following engagement with the Integrate Care Systems patient safety learning forums. Reduction of themed incidents reoccurring. |
| Deliver training to 85% of relevant managers on the review and feedback on incident reports through training in After Action Review processes and emphasising the importance of feedback on the incident reported. | Quality After Action Reviews are pivotal to ensure that maximum learning outcomes are identified. Managers should be supported in providing quality feedback and learning from incidents. | At this time not all lead reviewers across the organisation are trained in the After Action Review processes which are a core part of the Patient Safety Incident Response Framework. | Delivery of training to 85% of relevant managers. We will see an improvement in identified learning themes, quality AARs being undertaken and allow for early identification of emerging themes and maximisation of trust wide learning. We will see standardised feedback across the organisation. |
How we will monitor progress: Monthly Board reports detailing Learning from Deaths data and through the Patient Safety and Experience Group with progress reported quarterly to the Quality Governance Committee
Responsible Lead: Dr Simon Walsh, Medical Director
Date of completion: 31 March 2026
Priority Two - Clinical effectiveness
| Priority | Why we have chosen this priority | What we are trying to improve | What success will look like |
|---|---|---|---|
| Using Artificial Intelligence (AI) to improve ‘job cycle’ time. (Pilot) | Aligning to the NHSE priority for utilising digital technology, this will enable live time capture of patient assessments both face-to-face and through telephone triage (Hear and Treat) with the aim of; - Reduced on scene times which should impact on our ‘job cycle’ time, and in turn, our ability to respond to our C2 patients in a timelier manner, - Standardised documentation on patient care records - Accurate capture of patient assessment - Improvement in patient experience and safe care of patients. | On scene times which should impact on our ‘job cycle’ time, and in turn, our ability to respond to our C2 patients in a timelier manner, standardised documentation on patient care records, accurate capture of patient assessment. Improvement in patient experience and safe care of patients. | Pilot will enable comparison of job cycle time for instances where AI is used and not used. Strengthened documentation for any legal cases which should reduce closure time frames. (baseline to be determined in Q1 with the aim of a 5% reduction by year end). Positive feedback from clinicians – to be measured through a survey. |
| Pain management | Pain management is an important part of care and referred to as "the fifth vital sign". Managing pain can reduce stress, blood pressure, and heart rate, and positively affect healing. Pain scoring, which is essential to determine the impact of actions/treatment, is consistently one of the lowest performing indicators within the monthly Patient Care Record Quality audit. Following incident trends within 2024/25, management of pain has also been identified for a thematic review within the coming year. | Documentation of pain scoring to determine how effective any actions taken or treatment provided has impacted on the patient’s condition. | An increase to 95% (from 79-86% within 2024/25) of the documentation of pain scores monitored through the monthly PCR Quality audit. Clinical audit of abdominal pain included within the annual clinical audit plan. Thematic review undertaken by the Patient Safety team. |
| Inclusion of Glasgow software on all Corpuls monitors | Acting on findings from EEAST’s thematic review of cardiac patients and building on the NHS priority for utilising technology, this will provide automated interpretation of the ECG to support clinicians in identifying STEMIs, ensuring that patients are conveyed to a PPCI centre at the earliest opportunity. | Improvement in the recognition of STEMI patients to be conveyed to PPCI centres for definitive care. | Improved recognition of STEMI patients leading to a reduction in incidents of patients not being conveyed to PPCI centres. |
| Embedding of clinical supervision | Introduced in 2024/25, it is essential that we now embed this across the Trust to ensure that staff caring for patients in the urgent and emergency care setting have the knowledge and skills they need to do their job effectively. | Increased opportunities for staff to achieve their full potential whilst meeting the organisation’s need to deliver individualised patient care. | 95% of all clinicians to receive a supervised shift within the year |
How we will monitor progress: Reported quarterly to the Quality Governance Committee via the Clinical Best Practice Group and to the Trust Board via the Integrated Performance Report.
Responsible Lead: Simon Chase, Chief Paramedic and Director of Quality Date of completion: 31 March 2026
Priority Three - Patient Experience
| Priority | Why we have chosen this priority | What we are trying to improve | What success will look like |
|---|---|---|---|
| Expand the analysis and reporting from the patient surveys program to include reporting of experiences by different demographic groups. | We recognise that patients have different needs and access a variety of our services including being treated at home. We also recognise that patients experience of our service may differ based on a variety of factors including geographical location, age, gender and ethnic background. This will enable us to understand their experiences and make changes to improve our future provision of care. | Valuable feedback from specific service users and more difficult to reach groups on their care and experience. | Reporting to PSEG and committees will contain survey data which breaks down patient experience into demographic groups to identify a more accurate range of patient experiences. Identification of targets ways to improve patient experience for specific groups. |
| Ensure that education about changing services and clinical model is part of patient engagement | Work to engage patients and the public in the EEAST strategy development last year identified that many members of the public feel that they do not know enough about our services to feel that they can express an opinion on the strategy work. Current feedback from patients, including complaints and survey feedback also suggests that patients do not have a clear understanding of the range of services that the ambulance service now provides and of the different potential outcomes of calling the service. | Increasing public knowledge and understanding of our services will allow meaningful patient feedback and voice. | Patient engagement reports are able to demonstrate education around services and clinical model. Reporting into committees shows informed feedback around the range of services the Trust provides. |
| Expand CEG membership to include 16-17-year-old members to represent younger patients’ views. This will include developing all appropriate policies and processes to ensure the safety of younger volunteers. | We acknowledge that views of patients and their advocates is essential in improving experience and shaping our future to meet their needs. Initial broad demographic survey work suggests that young people aged 16-24 are some of the most dissatisfied with their experiences of care and treatment from EEAST. We need to ensure that all groups within our population are represented and that we nurture relationships with young people who can support us to understand and improve the experiences of our younger service users. | Increasing our engagement with patients and members of the public aged 16-24, increasing our understanding of their experiences and expectations to allow learning and improvement. | Appropriate policies and process in place to support volunteers aged 16-17 years old within EEAST. Recruitment of CEG volunteers aged 16 or 17. |
How we will monitor progress: Progress reported quarterly to the Quality Governance Committee and through the Patient Safety and Experience Group
Responsible Lead: Simon Chase, Chief Paramedic and Director of Quality
Date of completion: 31 March 2026
Part Three
- Performance of the Trust against quality metrics
- Clinical audit
- Participation in research
- Patient safety incidents
- Serious incidents
- When things go wrong
- Duty of Candour
- National Patient Safety Alerts
- Patient experience and feedback
- Patient and public involvement
- Raising concerns and Freedom to Speak Up
- Working with our local communities
- Commissioning for Quality and Innovation (CQuIN)
- Quality successes throughout the year
- Quality Governance Committee Assurance
- Statements from stakeholders
- Glossary
Progress on the quality account priorities 2024/25
The following section provides feedback and evidence on the progress of last year’s work on our key quality priorities and our performance.
The content is defined by NHS England and includes outcome results against specific indicators within five areas:
- Preventing people from dying prematurely
- Enhancing quality of life for people with long-term conditions
- Helping people to recover from episodes of ill-health or following injury
- Ensuring that people have a positive experience of care
- Treating and caring for people in a safe environment and protecting them from avoidable harm
Except for the time standards to our calls, no thresholds are set by the Department of Health for the Ambulance Clinical Quality Indicators.
Performance of the Trust against quality metrics
Response Times
Ambulance services are monitored against response times for a Category 1 – 4 system (determined by clinical condition/emergency), with varying response times for each category. The table below summarises the Trust’s performance against the national response time standards for 2024/25.
Although not meeting the national standards, except for the C1 (7 minutes mean and 90th centile) which was six seconds longer than the previous year, all categories were improved on the previous year with the exception of the C1 (7 minutes mean) which was six seconds longer than the previous year.
| Category | Definition | National standard | Average EEAST Performance 2023/24 and 2024/25 |
|---|---|---|---|
| C1 | Immediately life-threatening injuries and illnesses. | 7 minutes mean response time | 00:09:03 and 00:09:08 |
| 15 minutes 90th centile response time | 00:17:04 and 00:17:12 | ||
| C2 | Emergency. | 18 minutes mean response time | 00:43:51 and 00:42:49 |
| 40 minutes 90th centile response time | 01:35:56 and 01:32:50 | ||
| C3 | Urgent calls and in some instances where patients may be treated in-situ (e.g., their own home) or referred to a different pathway of care. | 120 minutes (2 hours) 90th centile response time | 05:03:57 and 02:21:56 |
| C4 | Less urgent. In some instances, patients may be given advice over the phone or referred to another service such as a GP or pharmacist. | 180 minutes (3 hours) 90th centile response time | 08:49:30 and 03:54:56 |
- Category C1 calls - maintained a consistent response time, averaging around 9 minutes across all months with a total average of 00:09:08.
- Category C2 calls - showed fluctuations throughout the year, peaking at 00:57:20 in December 2024 but averaging 00:42:42.
- Category C3 calls - had response times ranging from 01:39:49 to over 3 hours, with an overall mean of 02:20:51.
- Category C4 calls - consistently had the longest response times, exceeding 3 hours in multiple months, with an overall mean of 03:33:00.
March 2025 saw the best response times for the year for all categories.
- C1: 00:08:32 C2: 00:32:47
- C3: 01:38:57 C4: 02:30:00
Published further information for all ambulance services can be found here: www.england.nhs.uk/statistics and more detailed information relating to EEAST can be found within our Annual Report.
During the year, the Trust implemented several initiatives to enhance staffing levels and workforce effectiveness:
-
Recruitment and retention efforts: EEAST has successfully reduced staff turnover through a well-planned strategy, maintaining a strong workforce with valuable experience and skills, while saving on recruitment and external staffing costs.
-
Implementation of the 'Time for Me' wellbeing platform: In May 2024, EEAST launched 'Time for Me,' a platform powered by Hapstar, to support mental health and wellbeing. With nearly 700 employees and volunteers registered, over 60,000 wellbeing data points have been captured, enabling targeted support and early intervention.
-
Adoption of the NHS Long Term workforce plan: EEAST aligns with the NHS Long Term Workforce Plan, focusing on expanding education, training and recruitment to ensure a sustainable and resilient workforce.
-
Implementation of E-rostering and effective job planning: EEAST utilises electronic rostering and effective job planning to ensure appropriate staffing levels, enhancing productivity and patient care.
Our Operational Improvement Plan contains further actions to improve our performance, these include but are not limited to;
-
Reduction of our job cycle time (JCT) – JCT represents the total time taken to assist a single patient. The shorter the time taken the more patients can potentially be assisted. The largest part of the JCT is typically the on-scene times and these are within our control. Reducing on-scene times is crucial for providing care that aligns with the standards of other UK ambulance services and ultimately benefits the patient.
-
Roll out of Organisational Information portal (OIP), This action allows the visibility of individual performance and is planned for rollout alongside a framework of performance appraisals. OIP has now been rolled out Trust wide and is monitored locally by the management teams and progress reviewed through the regular Organisational Performance Improvement Plan (OPIP) meetings.
-
Education programme on clinical best practice on scene decision making. Led by the clinical leads, this education programme is designed to support staff outside of the normal on scene time ranges. All sectors have produced plans to roll out education.
In January 2025 the Trust received a Regulation 64 notification regarding our response times to category two patients. Further information relating to this can be found within the CQC section of this report on pages 11-14.
One factor affecting our C2 performance is the number of service provision hours lost – this can be impacted by a variety of causes however the biggest impact on the ambulance service within this are delays in handing patients over at our hospitals.
A national standard of 15 minutes is in place for our staff to handover a patient to the receiving hospital, however it is recognised nationally that this has not been met during the year - the average time within our region for 2024/25 was over 38 minutes, however it should be noted that some months exceed this. For example, the average time to handover in January was over 50 minutes.
EEAST has implemented several strategies to reduce ambulance out-of-service times, ensuring quicker responses to emergencies:
Implementation of ambulance handover units
In collaboration with local hospitals, EEAST has introduced ambulance handover units to facilitate quicker patient transfers. For instance, at Southend Hospital, a 12-patient capacity unit was established to expedite handovers, allowing ambulance crews to return to service more promptly. This initiative aims to enhance patient care by ensuring timely medical attention and reducing ambulance turnaround times.
Automatic handover protocols
Working with our hospitals and Integrated Care Systems (ICS) we implemented the system led Handover 45 (HO45) policy in November 2024. This policy, implemented by EEAST and other ambulance services, aims to address delays in transferring patients from ambulances to hospital emergency departments (EDs). Under this policy, if a patient handover is not completed within 45 minutes, ambulance crews may leave the patient in a designated area within the ED, provided the patient is clinically stable. To date, there have been no significant or fatal harm cases reported.
Collaboration with healthcare partners
EEAST collaborates with regulators, commissioners, and hospitals to reduce handover delays. By implementing handover escalation protocols, the organisations work together to identify and address offloading issues promptly, aiming to accelerate care and minimise delays.
Alternative care pathways
To reduce unnecessary hospital admissions and alleviate pressure on emergency departments, EEAST has developed alternative care pathways. These initiatives include the Clinical Assessment Service, which manages a significant proportion of 999 calls through 'hear and treat' methods, providing advice, guidance, or signposting to other services without dispatching an ambulance. Additionally, partnerships with unscheduled care services and the establishment of a single point of contact for referrals to various community services have been implemented. Further information relating to ‘hear and treat’ can be found on the next page.
As well as the Section 64 notification, in January 2025, the Trust also received a Section 29A Warning notice which included concerns regarding our call ‘pick-up’ time and the number of staff within our emergency operations centres (EOCs).
To enable patients to be treated correctly, our Clinical Assessment Service (CAS) continues to develop to ensure that patients who call 999 are directed to the most appropriate care provider for their needs
Following an initial assessment some patients will be managed via our Hear and Treat (H&T) service, this process within ambulance services is provided by paramedics and nurses undertaking enhanced telephone assessments of patients to determine the most appropriate response, which can sometimes result in no ambulance being sent. In May 2024 8.7% of patients were treated through this service, in December 2024 this number had risen to 12% meaning that more ambulances were available for our sickest patients.
Described within last year’s report, C2 segmentation is now part of our business-as-usual process with ongoing work ensuring that as many C2 patients are clinically validated as possible. The number of C2 calls reaching a H&T outcome has averaged between 4% and 6% throughout the year.
Each Integrated Care System (ICS) within the east of England has a functioning Unscheduled Care Coordination Hub (UCCH). Recruitment within each UCCH has resulted in an EEAST clinician co-locating with a multi-disciplinary team within each system every day. This ensures that patient demand of less urgent patients can be managed by the most appropriate community provider. In 2024, a total of 46,864 calls were passed via our Access to the Stack process. Of these, 33,503 (71.5%) were accepted by the community provider for initial management of the patients’ condition (either by telephone or face to face assessment). By working with our partners and allowing them to access our systems supports the Trust’s CAS staff to be able to validate other calls, such as those within the C2 category.
Recruitment within the CAS team has continued throughout the last year. There are now: 113 clinicians,11 clinical workforce managers and 25 clinical navigators all in post, ensuring that that the appropriate structure is in place to provide consistent support to the team and enact the processes to achieve H&T.
Over the next year, the ambition is to increase H&T within the team to 19%. Enablers for this include a continued focus of productivity within the CAS team and ensuring that system collaboration is increased for access to patient pathways.
Heart attack care
Coronary heart disease (CHD; also known as ischaemic heart disease) is the most commonly diagnosed type of heart disease. It is the most common cause of heart attack and is the single biggest killer of both and men and women worldwide. It's also the single biggest premature killer (before the age of 75) in the UK.
As many as 100,000 hospital admissions each year are due to heart attacks. Because of the life-threatening risk with a heart attack, providing patients with a pre-hospital assessment for an ST-elevation myocardial infarction (STEMI) heart attack and administering an appropriate care bundle means a significant improvement on patient outcomes, thereby supporting the NHS to reduce the number of patients dying prematurely and to help people to recover from episodes of ill-health or following injury.
STEMI care bundle
The mandatory quality indicator for ambulance services relating to this topic is the provision of an appropriate care bundle; recording of two pain scores, giving aspirin to break down the clot, giving glyceryl trinitrate (GTN) to dilate the coronary arteries and providing pain relief. The patient care record is audited against all these criteria and deemed to be either compliant or non-complaint.
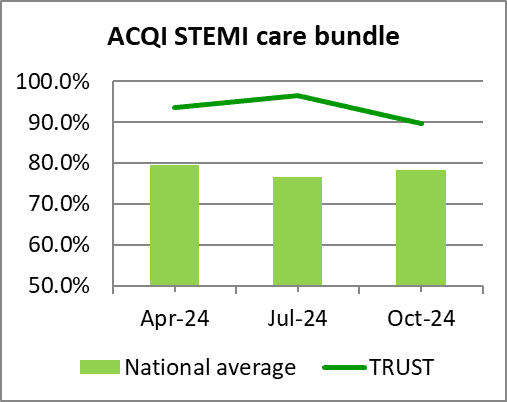
The data is reported on quarterly within the year and the table below shows our result against the national average and the best and worst scores achieved by ambulance services within England.
To provide a robust comparison, the table shows our achievement against the average and upper and lower compliance levels for ambulance trusts that have been published to date (April - October 2024). The graph demonstrates our performance against the national average data for each quarter (April - October 2024), both demonstrating that the Trust is well above the national average for each quarter within the year.
Achieving an average of 93.2% for the year to date, EEAST was the second highest performing Trust for this care bundle achieving 15.0% above the national average.
National data (April to October 2024)
| Heart attack care | National average | Upper | Lower | EEAST |
|---|---|---|---|---|
| STEMI Care Bundle | 78.2% | 96.1% | 58.2% | 93.2% |
Patients conveyed to a Primary Percutaneous Coronary Intervention (PPCI) Centre
Although the time it takes to transport a STEMI patient to a specialist Primary Percutaneous Coronary Intervention (PPCI) treatment centre is not a quality metric for the Quality Account, we report our achievement on a month-by-month basis to both NHSE and our commissioners. This ACQI contains two joint indicators for ambulance trusts and these centres both of which are measured in hours and minutes.
The table below shows our result against the national average and the upper and lower levels achieved by ambulance services within England for data published to date (April – November 2024). It should be noted that the lower score is the best performing score within these outcomes.
Latest data available April – November 2024 hh:mm
| Heart attack care | National average | Upper | Lower | EEAST Performance |
|---|---|---|---|---|
| Mean average time from call to catheter insertion for angiography | 02:30 | 02:55 | 02:20 | 02:33 |
| 90th centile time from call to catheter insertion for angiography | 03:32 | 04:02 | 03:07 | 03:35 |
As shown in the table above, EEAST performed just outside the national average for both of these measures, however we performed significantly higher than the lowest trust.
But, as demonstrated in the previous section, all patients received excellent care, with EEAST consistently achieving high compliance for the STEMI care bundle and being the second highest performing trust within the year.
Next steps
As well as continually being monitored through the national ACQI programme, one of the Trust’s ongoing priorities is to reduce our response times to Category 2 calls which include STEMI patients. This will be supplemented by a local priority for reducing the time spent on scene with these patients which will be monitored through a quarterly audit.
Stroke care - timeliness
Patients who are cared for in a defined stroke unit with organised stroke services are more likely to survive, have fewer complications and return home and regain independence quicker than patients on a general medical ward.
Although the time it takes to convey a stroke patient to hospital is not a quality metric for the Quality Account, we report our achievement on a month-by-month basis to both NHSE and our commissioners. Our performance is assessed monthly against three indicators for this ACQI: the mean average, median and 90th centile times from call to hospital arrival.
The table below shows our result against the national average and the upper and lower levels achieved by ambulance services within England for data published to date (April – September 2024). The Lower level relates to the best performing trust for this outcome. Unfortunately, national data reporting from NHS England has paused due to a delay in the implementation of the new Sentinel Stroke National Audit Programme (SSNAP) web tool for submissions so the Trust is unable to benchmark itself against the national average since September.
It should be noted that not all strokes are identified at the time of the call due to the information provided to the call taker, or the patient may deteriorate before or after the crew arrive.
National data – April - September 2024 hh:mm
| Stroke care | National average | Upper | Lower | EEAST |
|---|---|---|---|---|
| Mean average time from call to hospital arrival | 01:32 | 01:46 | 01:19 | 01:36 |
| Median time from call to hospital arrival | 01:20 | 01:32 | 01:10 | 01:23 |
| 90th centile time from call to hospital arrival | 02:23 | 02:45 | 01:58 | 02:29 |
On average EEAST performed outside the national average for all indicators for this period.
Next steps
As well as continuing to be monitored through the national ACQI programme, one of the Trust’s continuing priorities is to reduce our response times to Category 2 calls which includes stroke patients. This will be supplemented by a local priority for reducing the time spent on scene with these patients which will be monitored through a quarterly audit.
Cardiac arrest care
A cardiac arrest occurs when the heart suddenly stops pumping blood around the body. Someone who is having a cardiac arrest will suddenly lose consciousness and will stop breathing or stop breathing normally. Unless immediately treated by cardio-pulmonary resuscitation (CPR) and early defibrillation, this always leads to death within minutes. It is, however, possible to survive and recover from a cardiac arrest if you get the right treatment quickly. Around two-thirds of cardiac arrests outside of hospital happen in the home, but nearly half of those that occur in public are witnessed by bystanders. With each minute that passes in cardiac arrest before defibrillation, chances of survival are reduced by about 10%.
Although the indicators displayed in the table below are not quality metrics for the Quality Account, we report our achievement on a month-by-month basis to both NHS England and our commissioners, the exception being the post-Return of Spontaneous Circulation (ROSC) care bundle which is a quarterly requirement.
The post-ROSC care bundle contains six components, the recording and administration of: 12 lead ECG; blood glucose; end tidal CO2; oxygen; systolic blood pressure, and saline fluids for all patients who achieve a ROSC on scene which continues to hospital. Patients who had suffered a traumatic cardiac arrest, were successfully resuscitated before the arrival of ambulance staff or were aged less than 18 years are not included.
The table below shows our result against the national average and the upper and lower levels achieved by ambulance services within England for data published to date (April – November 2024).
National data – April – November 2024
| Cardiac arrest care | National average | Upper | Lower | EEAST |
|---|---|---|---|---|
| Return of Spontaneous Circulation (pulse) at hospital– All patients | 27.9% | 31.1% | 19.8% | 30.0% |
| Return of Spontaneous Circulation (pulse) at hospital – Utstein patients | 51.0% | 61.8% | 16.7% | 53.0% |
| Survival to Discharge – All patients | 10.2% | 13.0% | 8.2% | 9.4% |
| Survival to discharge – Utstein patients | 29.8% | 38.1% | 22.8% | 32.4% |
| Post-ROSC care bundle | 83.1% | 97.3% | 75.6% | 97.3% |
Next steps
This will continue to be monitored through the national ACQI programme. Successful outcomes from cardiac arrests are, in part, due to actions taken by acute organisations following arrival at hospital as well as early access to treatment and intervention. As our response times improve, so should our rates of ROSC and survival.
With the exception of 30-day survival (all patients group), EEAST is performing above the national average for all cardiac arrest related indicators. We were the highest performing average compliance for the Post-ROSC care bundle and 14.2% better than the national average for the time period. It should be noted that not all ambulance trusts submitted full data, so these outcomes must be used with caution.
Achievements against local priorities set for 2024/25
Priority One: Patient Safety
Shared judgement reviews under the Learning from Deaths programme
Building on the progress achieved within 2023/24, our aim was to continue to enhance our review process to incorporate a minimum of 40 shared judgement reviews per quarter. As shown within the table below, EEAST exceeded this target with a total of 400 completed within the year.
| Quarter 1 | Quarter 2 | Quarter 3 | Quarter 4 | Total |
|---|---|---|---|---|
| 44 | 119 | 69 | 168 | 400 |
Themes
The majority of cases showing a lower score were linked with delays which are managed via our approved system delays process and linked with our Organisational Performance Improvement Plan (OPIP), specifically regarding handover at hospital < 45 minutes and ongoing engagement with our ICB partners through the Urgent and Emergency Care (UEC) forums within each of our six sectors.
Our care in relation to resuscitation scored highly as also demonstrated within our Post-Return of Spontaneous Circulation audit outcome results, however a few cases were discussed at panel which has led to a PSII regarding resuscitation decisions to be included within this year’s Patient Safety Incident Review Framework (PSIRF) plan for 2025/26.
Improvement themes centre around poor documentation were also highlighted for which learning articles have been shared within our Safety Matters publication.
A further point of learning has identified that the processes around data collection and structured judgement reviews need to be developed to ensure that themes of improvement and excellence can be clearly identified, particularly regarding an automated reporting process within the dedicated mortality module in our Datix system and the creation of feedback pathways to staff.
Next steps
To further embed this process, this topic has been included as a priority for the coming year with two key objectives;
- A functional and fully automated mortality module to streamline the LFD process and effectively record data.
- Staff gaining feedback on LFD reviews in a timely manner to maximise learning across the organisation (reporting of number and timeframe for feedback).
Patient Safety Incident Response Framework
The Patient Safety Incident Response Framework (PSIRF) is mandatory for all services provided under the NHS Standard Contract including ambulance services and is in place to support the development of an effective patient safety incident response system in the NHS.
Whilst investigations into patient safety incidents are a part of the process, PSIFR looks to a broader approach with respect to patient safety, creating a shift to use of a range of learning response tools focusing on:
- compassionate engagement and involvement of those affected by patient safety incidents
- application of a range of system-based approaches to learning form patient safety incidents
- considered and proportionate responses to patient safety incidents
- supportive oversight focused on strengthening responses system functioning and improvement.
Our aim within the year was to continue to embed the Framework within EEAST following implementation in October 2023.
PSIRF is now well embedded in the organisation with the patient safety team completing two thematic Patient Safety Incident Investigation (PSII) reports since going live and will be completing a third in April 2025. The reporting of PSIRF and its effectiveness has been reported via the Compliance and Risk Group, Quality Governance Committee as well as the Executive Clinical Group. In addition to internal reporting the Head of Patient Safety reports regularly to the Integrated Care Board (ICB) colleagues across the region and the National Ambulance Risk and Safety Forum. The feedback gained from the work undertaken since adopting PSIRF has been extremely positive and has led to national learning following the Patient Safety Incident Investigation in relation to non-conveyance at EEAST.
Next steps
Although this will not continue as a priority in the coming year, the process will continue to be used to inform learning and two further priorities have been set to drive this important area of our work. In 2025/26 we are committed to enhancing the way in which we share learning from incidents, complaints and claims and ensuring that managers are fully trained in the After Action Review Process as detailed on the following page.
After Action Review Process
Within the Patient Safety Incident Response Framework (PSIRF), quality After Action Reviews (AAR) are one of the methods recommended for learning from patient safety incidents to ensure that maximum learning outcomes, including those that are positive, are identified.
Our aim within 2024/25 was to train band 7 managers within the organisation in the AAR process to drive improvements in identified learning themes, quality AARs being undertaken and to allow for early identification of emerging themes.
Leadership training is now a key component within our development programme and in line with our workforce plan, commenced roll out within the year. To date all Band 7 leading operational managers who have attended the ‘kickstart’ courses have been trained in this topic, as well as recently appointed local clinical managers, sector clinical leads and members of the patient experience and legal teams.
Next steps
The aim over the next 12 months is to train 85% of band 7 managers within the clinical operations directorate in after action reviews and this has been set as a priority for 2025/26.
Priority Two: Clinical effectiveness
Reduction of on scene times for STEMI and stroke patients
Pressures seen on system networks within our region continued to impact on our response to patients, particularly those coded as requiring a category 2 response (those that are classed as an emergency for a potentially serious condition that may require rapid assessment, urgent on-scene intervention and/or urgent transport). To ensure that our STEMI (heart attack) and stroke patients receive optimal care, it is important that we respond as quickly as we can and improve our overall ‘job cycle’ time for STEMI patients being conveyed to a Primary Percutaneous Coronary Intervention (PPCI) and stroke patients being conveyed to the nearest receiving hospital.
One of the actions within our Organisation Improvement Performance Plan (OPIP) is to reduce the amount of time that our clinicians spend on scene, a component within the ‘job cycle’ time.
In 2024/25 we re-introduced audits for both STEMI and stroke patients on a quarterly basis to review the amount of time spent on scene. The table below shows the number of cases included within the audit for each topic and the average time spent on scene in hours, minutes and seconds.
| STEMI | Apr-24 | Jul-24 | Oct-24 | Jan-25 |
|---|---|---|---|---|
| Number of cases | 110 | 110 | 87 | 118 |
| Time spent on scene (Trust average) | 00:44:10 | 00:47:33 | 00:49:38 | 00:47:52 |
| Stroke | Apr-24 | Jul-24 | Oct-24 | Jan-25 |
| Number of cases | 506 | 531 | 493 | 522 |
| Time spent on scene (Trust average) | 00:30:22 | 00:31:19 | 00:34:15 | 00:33:58 |
Feedback is sent to each sector after each period relating to their respective results however, from the table, disappointingly it can be seen that there has been no reduction within these times throughout the year with the highest times seen in October.
Next steps
These audits will continue throughout 2025/26 with outcomes disseminated to all areas. Time spent on scene is also monitored through our sector accountability forums and the Organisational Performance Improvement Plan (OPIP), this will continue in 2025/26.
Safe discharge of patients left on scene
Despite the introduction of a safe discharge audit in 2023/24, there had been several incidents and negative patient experiences throughout the year. Within this priority we were aiming to improve safety netting of those patients who we did not transport to hospital following treatment.
Our aim was to undertake a review to provide a benchmark on which to improve within 2024/25 and a reduction in the number of incidents reported.
From 01 January 2022 to 30 September 2023, the Trust reported 27 serious incidents relating to non-conveyance. On 01 October 2023, the Trust reported patient safety events against the Patient Safety Incident Response Framework (PSIRF) and from this date until 31 December 2024, reported 20 events of a serious nature.
The theme of non-conveyance was reviewed within a patient safety incident investigation (PSII) in October 2024 with several actions undertaken following its completion.
- Sharing of the report internally with staff and reporting via our Quality Governance Committee (QGC) and Executive Clinical Group (ECG).
- Sharing of the report externally to the Integrated Care Boards (ICB) within the east of England and the National Ambulance Risk and Safety Forum (NARSF) which has led to very positive feedback and prompted a national learning approach to non-conveyance within the ambulance sector.
- Review of the safe discharge care bundle in line with recommendations contained within the PSII report. Feedback from the pilot area was very positive.
- Face to face engagement led by the patient safety team to all new starters to the organisation remains in place and we now attend training courses to deliver a patient safety session to all courses running internally for emergency care assistant (ECA), Newly Qualified Paramedics (NQP) and Emergency Medical Technician (EMT) courses.
- Communications have been circulated via our intranet, EAST 24 and Safety Matters publications, promoting the shared decision-making model and expectations of staff in line with policy and best practice.
- Our Patient Care Record (PCR) policy has been updated to include the safe discharge care bundle as a mandatory element for completion for patients not transported following treatment.
Since the review and publication of the report, the Trust has only identified one serious patient safety event relating to the non-conveyance of a patient.
Next steps
- The revised safe discharge care bundle is being adopted as an internal Key Performance Indicator (commencing in July 2025).
- Review of the Non-Conveyance and Safe Discharge Policy (May 2025).
- Ongoing monitoring of incidents in line with our patient safety processes.
Falls in older people non-conveyed
Our Clinical Strategy identifies that the demands on our services are increasing and recognises the need to respond differently in a more holistic and community focused way. It is recognised that 999 is often the first point of contact for a fallen person and responding to falls incidents account for approximately 20% of our emergency activity. Many falls result in no injury and can often be responded to using appropriate alternative pathways therefore reducing the requirement for our frontline resources. Our aim for 2024/25 was to optimise the use of alternative pathways for non-injury falls to ensure that patients receive a timely response and to ensure that for older patients who were left at home following a fall were assessed appropriately.
Fire and Rescue Service (FRS) falls collaboration background
Towards the latter part of 2023, EEAST collaborated with Fire and Rescue Service partners in Bedfordshire, Cambridgeshire and Essex to provide the Community Wellbeing Officer (CWO) programme. This aims to strengthen collaborative working with fellow blue light partners in line with one of the Trust’s goals to be excellent collaborators and innovators. This project was fully funded by EEAST with the desire to innovate and improve services for patients and the local community.
According to NHS England's "Going further for winter: Community-based falls response," falls present significant risks, especially in elderly populations. Long periods lying on the ground post-fall (over one hour) are associated with serious injuries, hospital admissions, and even long-term care.
EEAST's Community Wellbeing Officer (CWO) project, which collaborates with Fire and Rescue Services (FRS), aims to reduce these risks by addressing falls rapidly, providing appropriate interventions at the scene, and enhancing safety with preventative measures such as home fire safety visits
Achievements of FRS Falls Collaboration
The CWO model demonstrates cost-effectiveness and has been a clinical and collaborative success. The reduced arrival time and high percentage of cases closed without an ambulance attendance underline the efficiency of the CWO team in attending lower acuity calls resulting in both financial savings and improved patient care.
During the pilot project an additional patient facing capacity has been generated with over 8000 on duty hours being logged by CWO teams. The creation of this additional capacity means that backfill of Standby Points (SSP) has been undertaken along with C1 coverage being provided across areas that previously have been subject to delayed response times. When a CWO team is the nearest resource, they will also attend C1 calls and have arrived ahead of EEAST on 69% of C1 calls that they attend.
Out of the 177 C2 calls attended in Q3 by a CWO, 13.5% were closed without the need for EEAST back up despite the higher grade of call. In all C2 calls attended, CWO’s were first on scene for 91% of these so, while not ‘stopping the clock’ on a C2, a clinical review of patients has commenced providing increased safety and quality of care.
From evidence collected by FRS, 44% of lower acuity falls call attended also received a fire prevention activity delivered during the time the staff were on scene with 16% of these receiving a follow up visit. FRS states that in the majority, these are high risk vulnerable people that may not have been reached by FRS without this collaboration.
The project has been recognised externally for its innovation and collaboration, nominated and/or winning multiple national awards for best practice and excellence, both within the fire and health arenas with consistent positive feedback from external stakeholders such as police and fire commissioners and MPs.
Care bundle for falls in older people (>65 years) who are left at home.
Nationally recognised that falls are the leading cause of emergency calls in the over 65s and that falls in older people are associated with increased morbidity and mortality, a new national quarterly Ambulance Clinical Quality Indicator (ACQI) was introduced by NHS England within the year.
The objective of the ACQI is to ensure that patients aged 65 years and over who have a fall below 2 metres, (less than 10 steps) should receive a thorough examination to exclude missed traumatic injuries before being discharged at scene safely.
This ACQI is made up of five components, all of which must be completed for the overall care bundle to be compliant.
- Detailed physical examination documented (examination to include more than one assessment from: head, ribs, spine, hips, and skin integrity, history of falls recorded, description of events preceding fall recorded, 12 lead ECG assessment documented, and that postural hypotension has been assessed
The Trust was involved in the design of the care bundle and part of the pilot before formal implementation, this enabled us to promote to staff the bundle and reasons for introducing this, across the organisation via bulletins and podcasts ahead of the ‘go-live date of 01 June 2024.
The first reporting period (June 2024) showed that EEAST achieved a compliance level of 88.0%, a very high level when compared to the national average of 43.3%. EEAST’s performance has continued to improve since then with a compliance level of 95.3% achieved in December 2024. The following table shows EEAST’s performance against the latest national data published to date (April – September 2024), the national average for December will be published in May 2025. EEAST continues to be the best performing trust for this care bundle achieving 46.4% higher than the national average for the financial year to date.
National data – April – September 2024
| Falls in > 65 years – non-conveyed | National average | Upper | Lower | EEAST |
|---|---|---|---|---|
| Care bundle | 44.3% | 90.7% | 19.0% | 90.7% |
Next steps
Following support from EEAST’s executive leadership team, the CWO project has been extended for 18 months and will now be part-funded between EEAST and FRS colleagues. EEAST will continue to monitor the project’s progress and evaluate its success with FRS partners.
The Trust will also continue to monitor compliance with the quarterly care bundle to ensure the high level achieved to date is sustained.
Priority Three: Patient Experience
Patient survey programme
Our aims in 2024/25 were to;
- Gain valuable feedback from specific service users and more difficult to reach groups on their care and experience.
- Develop bespoke user-friendly survey forms for patients to provide valuable feedback on their care and experience, identification and removal of barriers to enable a more inclusive feedback process from all patient groups.
In addition to the continuous and urgent and emergency care (UEC) and patient transport service (PTS) surveys, twelve bespoke survey projects have been undertaken during 2024/25. Bespoke projects will vary in line with the Trust’s priorities and strategies. These projects are often co-produced with experts by experience to ensure people and our community are treated as equal partners in service design, development, and evaluation.
Surveys are now available in a range of formats, including a co-produced easy read survey to ensure a more inclusive and accessible feedback process for all. All surveys undertaken include an equality and diversity monitoring section as standard good practice, to enable the monitoring of satisfaction across each of the nine protected characteristics.
A range of bespoke surveys were introduced in 2024-2025, with a focus on admission avoidance schemes and patients who had received assessment/treatment within the home setting. Overall, 97.0% of patients who were cared for through this process have reported satisfaction and expressed support for such initiatives and pathways - with many thankful to have avoided the need for hospital admission and associated handover delays. Such feedback provides tangible evidence of satisfaction, effectiveness and outcomes whilst ensuring the patient voice is present in the development of potential new interventions and pathways.
In addition, the stroke video triage survey has continued to gather feedback from patients who received a pre-hospital stroke video virtual triage assessment. Survey feedback has been shared widely with a view to optimise the stroke pathway, ensuring timely, appropriate care and the best possible patient outcomes.
Such opportunities have successfully raised the profile of EEAST, placing the patient voice at the centre to evidence the efficacy of initiatives to refine services and to securing longer-term funding for wider implementation.
The Trust is committed to enhancing patient experience and ensuring equitable care across all demographics, including seldom heard groups. This year, greater analysis has been undertaken to break down survey feedback into demographic groups, to better understand variances in satisfaction. Initial analysis indicates lower satisfaction levels for our younger patients (16-34 year olds: 61.5%) when compared to older patient (over 75 year olds: 92.3%).
However, in breaking down data for demographical analysis, it became apparent that most survey feedback comes from older, white British patients. This is not reflective of all the communities we serve. Many respondents had chosen not to provide demographic information on race or sexuality, limiting our understanding of patient experiences across different groups.
Next steps
We are expanding our CEG membership to include 16-17 year old members to increase the representation of younger patients’ views and voices. We will also enhance analysis and reporting by demographic groups to better understand diverse patient experiences, whilst proactively engaging with seldom heard groups. In addition, the co-designed children’s survey will be available as a survey option to increase the patient voice and the learning we gain from our youngest service users.
Co-production and working with experts by experience will continue to be embedded as standard practice, placing our patients and communities at the heart of service design, development and evaluation.
Patient and Public Involvement (PPI) Strategy
Our aim for 2024/25 was to ensure that patient engagement and feedback is part of EEAST’s ongoing strategy with evidence of the patients’ voice throughout.
Lots of patients and members of the public were willing to talk to the ambulance service, with most of their comments being positive. Approximately 200 members of the public were engaged and discussed this work at in person engagement events and a similar number via email. In addition, focus groups and online “big” conversations were held, and the Community Engagement Group and other health and public partners were involved via multiple workshops.
It is positive to note that patient needs and wants were established as part of the foundations of the project and public feedback about clarity of the strategy is evident in the final version of the strategy.
However, many patients and members of the public felt unable to provide critique or constructive input into what the ambulance service should do over the next 5 years as they felt that they did not understand how the service worked beyond a blue light response. Those who were able to engage in the big conversations and workshops tended to have enhanced knowledge of health services either professionally, as volunteers or through supporting those in frequent contact with them.
Next steps
To ensure that the public and our patients can meaningfully engage in future discussions about service development, we will ensure that education about our changing services and our clinical model becomes a more integrated part of our patient and public engagement.
Community Engagement Group (CEG)
In 2024/25, our aim was to increase the number of CEG members overall and recruit from communities and demographic populations not represented by the CEG.
Within the year, we have recruited and onboarded four additional CEG members, mostly from geographical areas with poor representation. We have worked with the Volunteer Advisory Forum (VAF) to seek additional support and materials aimed at increasing CEG recruitment. We have received applications from three 16–17-year-olds wishing to join the CEG (in addition to the 4 already onboarded members). Work has also been undertaken this year with some of our most active CEG members aimed at increasing the level of engagement from the whole group.
Due to the natural turnover of CEG members, these new volunteers have ended up replacing outgoing CEG members rather than increasing the overall membership. Whilst there has been some progress with regards to diversity of members, the group continues to be predominantly comprised of older white British members.
Next steps
We are putting the final policy changes through committees in the first quarter of 2025-2026 to allow the CEG to take on volunteers aged 16-17 years old to represent younger patients’ views. We will develop appropriate induction programs and support for younger volunteers, in conjunction with our first younger volunteers. We will also be working with the Trusts Multi-Faith Network to try and increase representation from different demographic backgrounds onto the CEG throughout 2025-2026 and support increased engagement opportunities in harder to reach communities.
For more information on how we work with patients and their representatives, please see the Patient Experience section of this report.
Clinical audit
Clinical audit is a crucial part of the Trust’s strategy to improve health care to service users. The evaluation of clinical performance against standards or through comparative analysis, with the aim of informing the management of services, is an essential component of modern healthcare provision. It forms part of the Trust’s clinical governance arrangements helping to ensure safe and effective clinical practices.
During 2024/25, EEAST participated in 100% of all required national audits which for ambulances are those defined within the Ambulance Clinical Quality Indicator (ACQI) programme; stroke; cardiac arrest, STEMI and falls in older people were included earlier in this section. It also fully participated in the National epidemiology and Outcome from out-of-Hospital Cardiac Arrest (OHCA) registry study undertaken by the University of Warwick and is included as an audit within the Healthcare Quality Improvement Partnership (HQIP) annual programme, of which more information and the latest publications can be found at https://warwick.ac.uk;
Within the year ambulance services began undertaking a new quarterly ACQI for Falls in Older People (> 65 years) who were not conveyed. Further information and outcomes for this audit can be found in the Priority Three: Patient Experience section of this report.
Local Audits 2024/25
Undertaking audits in relation to the nationally mandated Ambulance Clinical Quality Indicators relating to cardiac arrest, stroke, STEMI and falls patients is a huge amount of work, however in 2024/25 we completed our annual audit plan in full including local audits prompted by several other drivers including incidents and patient experience, as well as those prompted as re-audits from the previous year. We also supported a number of clinicians with audits in relation to their master’s qualification.
The following table shows the audit topic, levels of compliance, identified areas requiring improvement and next steps to improve the quality of care we deliver.
| Topic | Metric 2024/25 | Compliance | Areas for improvement | Next steps |
|---|---|---|---|---|
| Febrile Convulsion | Audit appropriate assessment for children < 5 years based on the previous National Clinical Performance Indicator (NCPI). | High levels of compliance were achieved for 4/5 indicators with blood glucose the lowest score of 94% due to exceptions. | Substantial assurance of compliance achieved. | Substantial assurance of compliance achieved. |
| Mental Health – Section 136 Audit undertaken in response to the National introduction (June 24) of Right Care, Right Person | To determine the impact of EEAST resources and time due to local Police Forces in EEAST requesting Patient Conveyance to an appropriate mental health (MH) suite or emergency department (ED). | April 2024 - 99.1% of S.136 patients attended resulted in conveyance to an MH or ED facility. Of these calls, 87.7% were received from either the police or Health Care Professional (HCP). Documentation of Mental Capacity Assessment achieved 80.7%.October 2024 – 100.0% of S.136 patients attended resulted in conveyance to an MH or ED facility. Of these calls, 94.2% were received from either the police or Health Care Professional (HCP). Documentation of Mental Capacity Assessment achieved 69.2%, a decrease of 11.5% on the previous audit. | Documentation of mental capacity assessment on EEAST ePCR prior to conveyance. | Re-audit within 2025/26 with the aim of increasing the documentation for a mental capacity assessment to 85%. |
| Advanced airway/oesophageal intubation | Minimum of 95% compliance. | Monthly audit achieving above set metric with latest data (Jan-25) demonstrating 97.9% compliance. | Increase on monthly compliance would ensure reduction in risk to patients. | <p>Sustain this level as a minimum. </p> <p>Continuation of monthly audit with failures sent to relevant operational management team so that individual clinicians can be directly notified and supported to improve. </p> |
| Asthma – Re-audit | Increase overall care bundle compliance by 25% above the level obtained in the previous audit (64.0%) | Overall care bundle compliance – 10.5% | <p>Recording of a peak flow including documenting when the patient was unable to provide one was the reason for the very low compliance for the overall care bundle. </p> <p> It was discovered that during the Covid years, EEAST removed the peak flow element due to the high airborne risk it presented and had not been reinstated to staff or training school. Education have now reinstated this part of the assessment.</p> | Audit of the recording of a peak flow, or valid exception, to be undertaken within 2025/26 with an aim of achieving > 80%. |
Cardiac Registry trial audit
We have continued to work with the Essex cardiothoracic centre in relation to the East Cardiac registry trial who use our data for those patients who have suffered a cardiac arrest in the pre-hospital arena and are conveyed to hospital. This audit forms the basis for a pilot of the British Cardiovascular Intervention Society post-resuscitated pathway.
Next steps:
This will continue within 2025/26, and reports will be available at https://www.bcis.org.uk/audit-results when published later this year.
Quality of documentation
An improvement identified and required within previous audits was the quality of documentation, a topic also identified within complaints and incidents investigations.
As a result, EEAST began a monthly Quality of Patient Care Records (PCR) audit in June 2023. The audit is set against the minimum data standard requirements for ambulance services (21 indicators) and each area is required to undertake and submit data for 50 records each calendar month.
| 2023/24 | Apr-23 | May-23 | Jun-23 | Jul-23 | Aug-23 | Sep-23 | Oct-23 | Nov-23 | Dec-23 | Jan-24 | Feb-24 | Mar-24 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall compliance | 94% | 95% | 94% | 94% | 95% | 95% | 95% | 95% | 95% | 95% | ||
| 2024/25 | Apr-24 | May-24 | Jun-24 | Jul-24 | Aug-24 | Sep-24 | Oct-24 | Nov-24 | Dec-24 | Jan-25 | Feb-25 | Mar-25 |
| Overall compliance | 96% | 97% | 97% | 96% | 96% | 96% | 97% | 95% | 96% | 96% | 96% | 97% |
The table above shows that the Trust overall achieved high standards of documentation, however there are consistently three areas where further improvements could be made; the documentation of a second pain score to determine the impact of actions/treatments; the recording of the name and place of the educational establishment for patients of school/college age (a recommendation from Lord Laming’s report into the death of Victoria Climbié); the name of the person to whom the patient’s care was transferred. This is needed to ensure that in any subsequent investigations, the correct members of staff within all organisations are identified.
Next steps
This audit will be ongoing with results shared with all areas on a monthly basis.
The annual clinical audit plan will continue to be an integral part of monitoring and improving the quality of care delivered to our patients with work on the approved annual plan for 2025/26 already started.
Results are shared with staff across the organisation in the form of posters and podcasts, the introduction of supervisors and clinical managers within the organisation will provide an additional opportunity to share outcomes with staff to improve the quality of care delivered.
Participation in research
Clinical research is an important function within the NHS, bringing benefits to patients, clinicians, and NHS Trusts. High quality research activity provides evidence for new ways of delivering care, as well as preventing, diagnosing, and treating conditions. Many patients want to take part in research and study findings result in better treatment for them. Research-active Trusts tend to attract more forward-looking clinical staff, and their involvement in research helps them to understand research evidence and use it in their clinical practice.
The EEAST Research Support Service (RSS) works with academic and other health and social care partners regionally and nationally to develop, support, deliver and promote research as a core part of service provision. RSS ensures that patients and staff have a broad range of opportunities to participate safely in relevant pre-hospital ambulance research.
During 2024/25, EEAST recruited 363 participants (patients and NHS staff) into eight high quality research studies approved by Health Research Authority. All were eligible for the National Institute for Health Research (NIHR) Portfolio, and one, EVOLVED, was an EEAST-sponsored study:
- Medication route in cardiac arrest - PARAMEDIC3 (n=25)
- Exploration of behaviours and lifestyle factors impacting levels of vitamin D within a UK ambulance service workforce - EVOLVED (n=40; EEAST-sponsored)
- Randomised trial of paramedic delivered Fascia Iliaca Block (specialised pain management) for hip fracture - RAPID-2 (n=9)
- Intramuscular tranexamic acid for the treatment of symptomatic mild traumatic brain injury in older adults: a randomised, double-blind, placebo-controlled trial – CRASH-4 (n=25)
- Ambulance Response to Older Adults who have Fallen - a mixed methods study - AMBOFALL (n=43)
- Measuring Air Pollution from Ambulances – MAPA Pilot (n=167)
- Rapid Ambulance Diagnosis of Stroke: a pre-hospital feasibility study – RADIOS (n= 32)
- Frontline ambulance service staff cultural competence study (n=22)
Note: n= relates to the number of participants recruited into each project.
Further information is available by contacting RSS at research@eastamb.nhs.uk. EEAST has a reputation for successful development and delivery of high-quality research. Such continued participation in clinical research has demonstrated the Trust’s on-going commitment to improving the quality of care offered and contributing to wider health improvement
Patient Safety Incidents
A patient safety incident is defined as any unintended or unexpected incident which could have or did lead to harm for one or more patients receiving NHS care. This includes:
- incidents that caused no harm or minimal harm,
- incidents with a more serious outcome,
- prevented patient safety incidents (known as ‘near misses’).
The chart below shows the number of delay incidents vs the total number of patient safety incidents.
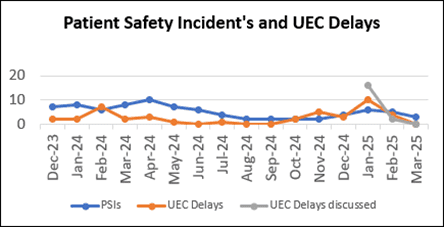
The number of incidents reported by staff during 2024/25 demonstrates a good culture of reporting and being open and honest. Where a near miss has happened, proactive steps can be taken to reduce the risk going forwards and to maintain a learning from incidents culture, the overall number of patient safety incidents relating to delays has decreased since 2022/23 as illustrated in the chart below. The charts below demonstrate our performance for both of these points.
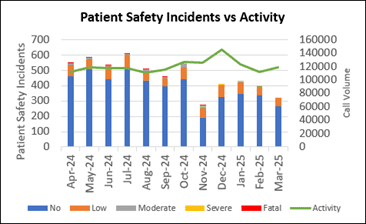
The second chart shows the number of patient safety incidents reported versus our activity during the year.
Prior to the implementation of the Patient Safety Incident Response Framework (PSIRF) EEAST reported on the level of harm they directly caused in relation to individual incidents. Since the implementation of PSIRF in October 2024, the parameters to which levels of harm are reported have been updated in line with Learning from Patient Safety Events (LFPSE) guidance to reflect how EEAST may have contributed towards harm.
A condition within the Quality Account requirements is for each Trust to provide a comparison of their patient safety incidents reported to NRLS against the national average for similar services. However, with this process moving to the new reporting platform, reports have been paused, and no data had been published for 2024/25 at the time of writing this document.
Serious Incidents
In 2023, the system used to report and monitor the progress of Serious Incident investigations across the NHS, transferred from the Strategic Executive Information System (StEIS) to a new reporting system, Learning from Patient Safety Events (LFPSE).
This is supported by a new Patient Safety Incident Response Framework (PSIRF) which makes no distinction between ‘patient safety incidents’ and ‘Serious Incidents’. As such it removes the ‘Serious Incidents’ classification and the threshold for it. Instead, the PSIRF promotes a proportionate approach to responding to patient safety incidents by ensuring resources allocated to learning are balanced with those needed to deliver improvement.
Within this framework, organisations are required to implement a plan that takes account of several categories including;
- the involvement of patient safety partners,
- engaging and involving patients, families and staff following a patient safety incident,
- responding proportionately to patient safety incidents,
- oversight roles and responsibilities,
- patient safety incident response standards.
Recording patient safety events, whether they result in harm or not, provides vital insight into what can go wrong in healthcare and the reasons why. At a national level, this allows for new or under-recognised safety issues to be quickly identified and acted upon on an NHS-wide scale, ensuring providers across the country take action to reduce the risk.
*The data in the table shows SI figures from 01 April – 30 September 2023, PSIRF data shows figures under the new framework which EEAST implemented on 01 October 2023.
| Category | 2023/24 * (SI data) | 2023/24 * (PSIRF data) | 2024/25 * (PSIRF data) |
|---|---|---|---|
| Delay | 36* | 24* | 29* |
| CAS / AOC | 7* | 4* | 11* |
| Patient injury | 1* | 1* | 5* |
| Clinical treatment | 2* | 7* | 12* |
| Non-conveyance | 4* | 13* | 7* |
| Equipment failure | 0* | 0* | 0* |
| Other | 4* | 0* | 15* |
| Total | 54* | 49* | 79* |
Never Events
There were no ambulance specific Never Events within the NHS Never Events List for 2024/25. It should be noted that Never Events formed part of the previous Serious Incident Framework, with the implementation of PSIRF, NHSE is currently consulting on a new Framework.
When things go wrong
It remains important to us to act in a timely manner when something goes wrong. This part of the report shows the response we made in acting on some of these things and what we did about them following the reporting of an incident.
| What went wrong | What we did | What this means |
|---|---|---|
| An increase in incidents being raised in relation to the failure of Mangar Elk cushions (an emergency lifting cushion used to lift a fallen person). | Proactive work with our medical devices group has led to a long-term solution being implemented across the Trust | The Trust has seen a reduction in reported incidents in relation to Mangar Elk failures, in Q4 there were no Mangar Elk issues reported. This has led to an improvement in care of those patient we attend who have fallen. |
| The number of shared judgement reviews being completed under the Learning from Deaths framework was lower than anticipated. | We identified that we required more clinicians trained to complete the Structure Judgement Review (SJR) process. An additional 21 clinicians are now trained in facilitating SJRs | During 2024/25 compliance has been exceeded each quarter. In total the number of SJR’s completed for 2024/25 is 400 as of the 31 March 2025 |
| A regular PTS patient was being transferred in a wheelchair and unfortunately, due to the pavement being obstructed by cars, the wheelchair got caught and the patient was tipped out of the chair. The patient was taken to his out-patient’s appointment; however, we received a subsequent 999 call. Due to pressure delays it was a further 2 and ½ hours before an ambulance arrived to convey him to A&E. | Identified that the member of PTS staff had not followed the correct procedure in relation to immediately dialling 999 if a patient sustains an injury in their care. The procedure and associated video were circulated to all PTS staff via the PTS newsletter and staff emails. In addition to the above a Patent Safety Incident Investigation is underway led by the Patient Safety Team and will be completed by April 2025 | Staff reminded of the actions to take when a patient is fallen. A further action related to the reassessment of a patient’s mobility when concerns are raised or when a patient has regular journeys. Both of these actions should reduce the risk to patients. |
Duty of Candour
NHS providers have a statutory duty to inform and involve patients and their families in investigations where there has been severe harm under Regulation 20 of the Health and Social Care Act. In line with our policy, Duty of Candour (DoC) is overseen by the Patient Safety team and is attempted to be discharged for every serious incident, regardless of the level of harm caused. Further relevant cases are identified through a daily review of incidents reported. Contact is made with the patient, or a nominated representative, via telephone in the first instance. Following the primary telephone call, the conversation is summarised in a letter.
The content of our primary Duty of Candour conversations include:
- An introduction.
- An explanation of the incident identified.
- A sincere apology from us and condolences if the patient has sadly died.
- An explanation of the investigation process.
- An opportunity for the patient or nominated representative to ask any questions which they would like to be answered in the investigation.
- Establishment of preferred methods and frequency of involvement and communication throughout and after the investigation period.
Although Regulation 20 of the Health and Social Care acts requires the Duty of Candour to be discharged as soon as is reasonably practicable but always within 10 working days, there are often instances when it takes us longer to identify the individual most appropriate to discharge the Duty of Candour to.
This is due to us not always having full patient or next of kin information. Our approaches to finding out this information include:
- communication with GPs,
- liaising with the patient safety specialists at the admitting hospital and
- close working relationships with His Majesty’s Coroners.
Analysis of our data demonstrates the following compliance with Duty of Candour for 2024/25 for serious incidents and Patient Safety Incident reviews compared to the previous three years.
| 2021/22 | 2022/23 | 2023/24 | 2024/25 | |
|---|---|---|---|---|
| Number of cases initially requiring Duty of Candour | 161 | 277 | 112 | 78 |
| Duty of Candour discharged | 161 | 272* | 109* | 53* |
| Average timeframe for DoC to occur (working days) | 4.5 | 4.0 | 6.0 | 7 |
| Average timeframe for letter follow-up (working days) | 1.7 | 1.0 | 1.0 | 1 |
- For cases where Duty of Candour was not discharged, this is due to not being able to identify or make contact with next of kin despite best efforts to do so.
National Patient Safety Alerts
Patient safety issues that require national action are identified predominantly through incidents reported by providers to the National Reporting and Learning System. When these issues are identified, work is undertaken with frontline staff, patients, professional bodies, and partner organisations to decide if there is a large enough risk to issue a National Patient Safety Alert (NPSA) through the Central Alerting System, which in turn sets out actions that healthcare organisations must take to reduce the risk.
These alerts must be acknowledged and, where appropriate, actions taken.
The Trust has a robust way of monitoring compliance with national alerts and this year following review, none were deemed to be relevant to EEAST or the ambulance sector.
Patient experience and feedback
Although not mandated to report on patient experience, as a Trust we feel that it is important to tell people how we are continually developing and improving our services as a result of our patients’ experiences and feedback. Patients are at the heart of everything we do and as such we believe that the patient voice should be a key driver in the way that we improve our services. The following pages provide information on what our patients and their families have told us through public engagement, complaints, concerns, compliments and surveys, what steps we have taken to improve and how we intend to improve further in the future.
The Patient Experience Team co-ordinate complaints, concerns, compliments and comments as well as leading proactive patient and public engagement for the Trust, in line with the NHS Complaints Regulations 2009, the Public Health Ombudsman Complaints Framework, and local policy. All feedback, both positive and negative, is managed and recorded by the department. Communication with patients or their families is maintained throughout the process, and they are provided with a response to their feedback, with a focus on resolving complaints and identifying learning from both complaints and compliments at the earliest opportunity.
Compliments
Compliments always far outweigh the number of complaints received and in 2024/25, 3,931 compliments were reported to the Trust, which equated to an average of 328 per month (meaning that the average monthly compliments received has consistently increased year on year for the last 3 years). The Trust received four compliments for every complaint received this year (this appears lower than last year due to changes in the way that the Trust now records complaints as described below). Compliments are reported to the Trust board and the individual colleague and are recorded on the staff member’s personnel file. This year we have started looking at themes from compliments to help us learn from excellence, and the common themes include professionalism, kindness and being calm and reassuring.
| Apr-24 | May-24 | Jun-24 | Jul-24 | Aug-24 | Sep-24 | Oct-24 | Nov-24 | Dec-24 | Jan-25 | Feb-25 | Mar-25 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Compliment | 365 | 331 | 280 | 382 | 331 | 358 | 296 | 296 | 305 | 317 | 293 | 377 |
| Complaint | 89 | 69 | 90 | 103 | 84 | 74 | 79 | 72 | 50 | 47 | 55 | 44 |
Complaints
As a Trust we closely monitor the numbers and themes of complaints that we receive and use this learning to support service improvement. During 2024/25, in order to comply with the Public Health Ombudsman Complaint Framework Guidelines, expressions of dissatisfaction ceased being categorised into complaints and concerns, with all being recognised and reported as a complaint. This means that the overall number of complaints this year is higher than previous years at 868, however when compared to the total number of complaints and concerns combined last year, we see a reduction.
Complaints arose from 0.05% of our contacts with patients which is a sustained improvement of 0.1% on the previous year. All complaints which cannot be resolved under early resolution receive a local investigation and depending on the nature of the complaint or concern, may also be reviewed by the patient safety team. Complainants are supported through the process of raising a complaint and investigation by our patient experience coordinators, and upon receiving a written response, face to face meetings are arranged where complainants require further support. An anonymous sample of our complaint responses is reviewed by the Trust volunteers from the Community Engagement Group and feedback is provided to the patient experience team to ensure improving quality of complaints.
The number of re-opened complaints remains very low (1.2% of all complaints responded to this year), meaning complainants are usually satisfied that our responses have addressed and where able, resolved their questions and concerns.
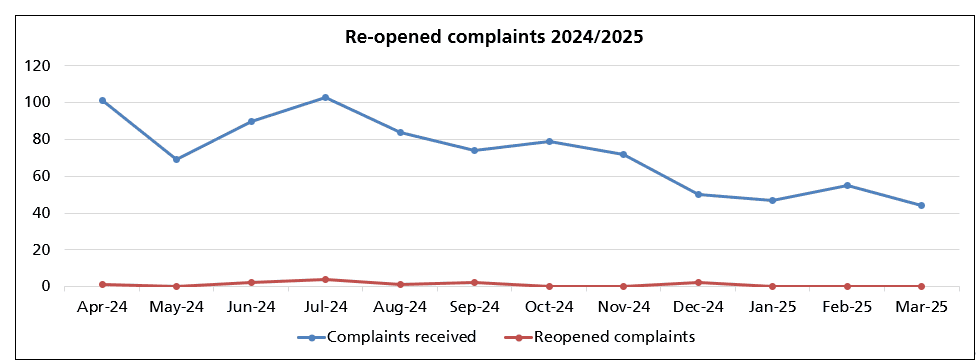
Graph showing the number of compliments and complaints received each month during the year.
The biggest theme from complaints and concerns was delay, with most of those complaints (62%) being related to The Patient Transport Service (PTS) rather than Urgent and Emergency Care (UEC) service or our Emergency Operations Centres (EOC). The next biggest themes were transport and driving (88% of these complaints were for PTS), attitude which largely related to the Trust’s UEC service (76% of complaints were for our UEC service), and clinical assessment and treatment (which by nature relates almost entirely to our UEC services and emergency operations centres). It is of note that although the themes of complaints remain the same, progress is demonstrated by the reduction in numbers of complaints received in most of these areas. Delay complaints were reduced by 30% compared to 2023-2024 with reductions in all services but the most significant reductions for PTS. Similarly transport and driving complaints were reduced by 12% compared to the previous year, with the reduction almost entirely in PTS. Clinical assessment and treatment complaints, which largely relate to UEC services and EOC decreased by 21% on the previous year.
These reductions in complaints represent improvements in emergency ambulance attendance times achieved via the Trust’s delay action plan and in the last quarter of the year, through interventions such as the implementation of handover in 45 minutes with local acute hospitals. Regarding clinical assessment and treatment, reductions in complaints are likely to also reflect an increase in admission avoidance schemes, increased out of hospital treatment options and pathways and internal learning from Patient Safety Incident Reviews. For the patient transport service, reductions in complaints are the likely result of improvements to their planning and prioritisation of service delivery as well as the cessation of one of their most over utilised contracts.
Parliamentary and Health Service Ombudsman (PHSO)
Although most complaints are successfully resolved through the Trust’s complaints process, complainants can refer their complaint to the Parliamentary and Health Services Ombudsman (PHSO) for an independent review. This happens if a complainant feels that their complaint has not been resolved, and the Trust has exhausted all avenues of resolution. This provides complainants with an impartial, independent review of their complaint and gives clear guidance to the Trust on how to improve our investigations and responses.
In 2024/2025 the Trust was not notified of any cases which had been referred to the PHSO by complainants. We do still have complaints in initial review from 2023/2024, although the Trust has not yet received initial feedback indicating whether these will move to an investigation. The Trust was notified this year that the PHSO did partially uphold two complaints from 2023/2024. Given the length of time since these complaints had been made, the Trust had already implemented learning by the time that the PHSO notifications were received.
You said, we did
As a Trust we recognise the importance of learning when things have not gone as well as we would have liked or from our patient survey feedback. The following case studies are just three examples of some of the learning from last year.
| You said | What we did | What this means |
|---|---|---|
| We were receiving frequent complaints that our Patient Transport Services were cancelling lots of appointments at the last minute, and that patients felt that organisation was poor. | We invested in upgraded software which allows the control room to plan journeys six weeks in advance. The letters to patients who have experienced delays and cancellations have been worked on to include information about the challenges that the service is facing and the agreements for prioritising patients where demand exceeds capacity. | Where journeys have been over booked, in most cases patients have sufficient time to make alternative transportation arrangements rather than having to cancel their appointments. Where patients have still had poor experiences, our letters are more transparent about the challenges facing the service, the plans in place to reduce these and what this may mean for their care. |
| Patient feedback from the Stroke video triage project said that patients were pleased to have received a video triage assessment and with the outcome of this. | As a result of this and staff feedback, we have worked with local hospitals to increase the times that this is available and to implement stroke video triage in more hospitals. Survey feedback has been shared nationally and internationally as part of ongoing research into stroke video triage. | More patients within EEAST’s region will be able to benefit from the reduced arrival to images and intervention times that the stroke video triage project has already demonstrated. Patient feedback and EEAST’s work on this is contributing to improving the stroke pathway for the ambulance sector nationally. |
| Patients in the 16-24 age group have consistently said that they are less happy with the services that they receive from EEAST than other age groups. | We have amended our safeguarding policies, developed policies around parental involvement and explored solutions to practical barriers to allow 16- and 17-year-olds to volunteer for the Trust Community Engagement Group. | We anticipate our first 16- and 17-year-old volunteers being able to join the Trust in 2025. This will mean that this age group is better represented and has more opportunity to contribute directly towards service improvement. |
Patient surveys
As stated within a previous section, the Trust has a comprehensive annual patient survey programme which includes continuous surveys for the urgent and emergency care service (UEC) and the patient transport service (PTS).
Patient surveys are signposted using a variety of methods, including the Trust’s social media channels, invitation to feedback letters and patient information cards. In addition, 60.0% of PTS survey submissions received during 2024/25 have resulted directly from SMS signposting.
Listening to the patient voice enables the Trust to identify, not only what is working well, but also to highlight areas for learning and service improvement. Feedback received through surveys is monitored and triangulated with the themes identified through complaints, patient engagement, and patient safety to ensure appropriate governance, learning, and to improve patient experience and outcomes.
It also enables the Trust to identify areas of excellence and highlight areas for learning and service improvement. Feedback received through surveys is continually monitored and triangulated with the themes identified through complaints, patient engagement, and patient safety to ensure appropriate governance, learning and to improve patient experience and outcomes.
All patient surveys include the Friends and Family Test (FFT) question, ‘Overall, how was your experience of our service?’ The FFT is a method of calculating the overall satisfaction of the patient and is used as a benchmark across the Trust. The FFT result is calculated by dividing the proportion of ‘very good’ and ‘good’ responses (numerator), by the overall number of responses (denominator).
The FFT is a national directive, and the Trust is required to provide all PTS patients with the opportunity to respond to the FFT question, with results reported monthly to NHS England.
Outcomes from 2023/24 and 2024/25 can be found below. Historically, survey feedback demonstrated higher satisfaction levels for EUC patients, however, recent years have seen UEC and PTS patient satisfaction to have become more comparable.
Overall Satisfaction (Friends and Family Test)
| Continuous Patient Survey Results: | Number of patients: 2023/24 | Overall Satisfaction: 2023/24 | Number of patients: 2024/25 | Overall satisfaction: 2024/25 |
|---|---|---|---|---|
| Urgent and Emergency Care | 873 / 978 | 89.3% | 702 / 815 | 86.1% |
| Patient Transport Service | 1180 / 1401 | 84.2% | 1612 / 1865 | 86.4% |
| All Services | 2053 / 2379 | 86.3% | 2314 / 2680 | 86.3% |
Survey projects
This section provides further information on each of the surveys undertaken throughout the year.
Easy Read
The easy read survey (co-produced with the D.R.A.G.O.N.S at the Norfolk and Norwich SEND Association (NANSA) has remained available as an accessible survey option for UEC and PTS patients, empowering patients to provide feedback on their experiences to drive forward learning, improvement and informed decision making.
Feedback received during 2024/25 has generally been positive about the service and staff (overall satisfaction: 92.6%). Most patients felt listened to (96.2%), with staff communicating in an understandable way (98.1%), ensuring any sensory needs were met. The main area of dissatisfaction has related to ambulance and PTS delays, which has been shared as part of the ongoing wider system review.
This survey has highlighted the importance of co-production and working in equal partnership with experts by experience. Building on the co-production sessions, a short video was created to explain how to complete the survey and to outline how feedback is used. The video, which includes a British Sign Language (BSL) translator and voiceover (recorded by a NANSA D.R.A.G.O.N), is now available to view on the EEAST website.
Safeguarding
The safeguarding survey has continued throughout 2024/25, with the aim being to obtain feedback from patients who had consented to a safeguarding referral (e.g. mental health services, falls team, GP, local authorities and the Fire and Rescue Service).
Overall satisfaction levels have remained high (96.3%), with patients generally advising that they were included in discussions relating to their referral and support needs (88.1%).
Just under three quarters of patients surveyed (71.8%) went on to receive additional support post referral. Dissatisfaction has mostly related to delays and communication.
Patient feedback received has been utilised as an assurance tool, and during 2024/25, survey findings have also been shared within the CQC Joint Targeted Area Inspections of Hertfordshire County Council and Norfolk County Council, Safeguarding Adult Boards and Safeguarding Care Act audits across the region. EEAST has taken the lead in being able to demonstrate this level of engagement.
The safeguarding survey will be undertaken again during 2025/26 to measure impact on patient experience considering the impending changes relating to the introduction of electronic safeguarding referrals (via iPads rather than Single Point of Contact (SPOC) contact).
Maternity
The maternity survey has continued as an online option during 2024/25, enabling patients to provide feedback following their maternity related 999-emergency call.
Whilst patients have continued to mostly report a positive experience of the staff and service received (94.1%), several patients expressed dissatisfaction with the advice provided, prompting suggestions relating to additional obstetric training for both clinicians and call handlers. This has been shared with the maternity lead and specialist midwife to ensure learning and further training as required e.g. videos (such as for delayed cord clamping).
Stroke video triage
During 2024/25, the stroke video triage survey has continued to proactively seek feedback from patients who received a pre-hospital stroke video triage assessment, with this initiative in place to ensure timely, appropriate care and the best possible patient outcome. The pathway itself has had a positive impact on patient arrival to imaging time, alongside significant reductions in the treatment times for stroke at all live centres.
Survey feedback has also demonstrated that patients have generally been satisfied with the service received (80.4%) and pleased to have received a video triage assessment. The slightly lower than expected satisfaction level generally relates to many patients being unaware that an assessment had been undertaken using this method – promoting the need for improved communications. Aside from ambulance response times, areas for improvement also related to WIFI connectivity and the need to extend the availability of this virtual method.
Survey feedback has been shared widely, including NHS England, the Integrated Stroke Delivery Network, both national (UK Stroke Forum) and international (European Stroke Organisation Conference) conferences, and as part of ongoing research looking at the experiences of patients and caregivers involved in stroke video triage.
These opportunities have successfully raised the profile of EEAST, whilst evidencing the efficacy of the project to improve patient experience, outcomes and optimisation of the stroke pathway for the ambulance sector nationally.
Mental health
During 2024/25, two co-produced Instagram poll surveys relating to mental health have continued to obtain feedback from patients who had contacted 999 when experiencing a mental health crisis.
Whilst feedback has continued to demonstrate satisfaction with the service received from EEAST (between ‘good’ and ‘very good’ on the sliding scale), feedback continues to highlight the need for improved mental health support and signposting. In addition, approximately a quarter of patients have advised that they did not feel listened to or understood by the emergency call handler. Patients have also continued to stress the importance of only telling their story once.
The survey feedback has been shared widely to ensure 360 feedback, working with mental health practitioners, commissioners, partner organisations and experts by experience to ensure system wide learning and improvements to the service provided to patients.
As a result of patient feedback;
- further co-produced call handler engagement sessions are in development for 2025/26.
- 999 emergency pathway videos and infographics are now available on the public website.
- In addition, the summer engagement programme will focus on education relating to the clinical model and the importance of the right care, by the right person, at the right time.
Admission avoidance
This year has seen the undertaking of several admission avoidance related surveys, with a view to proactively obtain feedback from patients who received assessment/treatment within the home setting, with many avoiding conveyance to hospital.
Admission avoidance initiatives aim to ensure the right care, by the right person, at the right time – with survey feedback received demonstrating positive patient experiences and outcomes, with demand upon acute Trusts also reduced as a result.
Surveys have related to skin tear wound treatment, the Physician Response Unit pilot and the Advanced Practice Team. Patients have largely supported such models of care, with many thankful to have avoided the need for hospital admission and associated handover delays.
Areas of dissatisfaction have generally related to delays and communication, although these comments have been in the minority. In addition, it is clear from feedback received that patients are not always aware of/understand the range of services and possible outcomes following emergency call triage.
The collation of patient feedback provides tangible evidence of satisfaction, effectiveness and outcomes. This is crucial to refine services and secure longer-term funding and wider implementation post pilot. This year’s engagement programme will also focus on education relating to the clinical model and alternative pathways in place.
Next steps
The Trust is committed to developing its patient experience and engagement activity and continually explores new methods to obtain feedback and to ensure equity of care across the demographics, including seldom heard groups.
During 2025/26, there will be a focus on expanding the Community Engagement Group, with a view to diversify the group, and encourage younger engagement across the region.
Co-production and working with experts by experience will continue to be embedded as standard practice, placing our patients and communities at the heart of service design, development and evaluation.
In addition to the continuous surveys, the 2025/26 survey programme will include several planned projects, with a prioritisation on learning and improvement - ensuring incorporation of the Trust priorities and the Patient and Public Involvement strategic objectives. Key survey results and themes will continue to be reported as part of the internal and external quality and assurance reporting channels, ensuring the patient voice is at the heart of the organisation.
Patient and public involvement
Although we are not required to report on our engagement with our patients and their representatives, we feel that it is important to hold ourselves to account for how we engage our patients and the public and how we represent patient voice within the organisation.
Community Engagement Group (CEG)
The EEAST Community Engagement Group (CEG) has made notable progress in representing the patient voice during 2024/25. The CEG now have a regular place at Trust board meetings, presenting reports on their activities and having the opportunity to ask the Board questions quarterly embedding the link from Board level to the patients and public EEAST serves.
The members have assisted with numerous public engagement events and activities, complaints reviews, station IPC audits, undertaken patient discovery interview training, attended internal and external meetings to represent EEAST community engagement, contributed to the developed of the 2025-30 strategy and EEAST values, supported members of staff, and flown the flag for the patient and public voice at EEAST brilliantly.
Following a coproduced review of the structure of the group in 2023, the group continues to embed this revised approach which provides greater accessibility and opportunity for people to participate in community engagement volunteering at EEAST in ways that meet their capacity to volunteer. Core members of the group working in collaboration with the Patient and Public Involvement Team, have focussed on ways to increase engagement from members and help drive the group forward.
As reported previously within this document, a key area of focus has also been to extend the group to welcome 16-17 year olds to the group with work taking place to look at appropriate safeguarding and engagement opportunities for this age group. We look forward to officially welcoming the first 16-17 year olds into the group during 2025.
Engagement Activities
Face to face engagement events provide an opportunity to meet with the public and gain feedback from people who may not usually have contacted EEAST. It also provides an opportunity to provide education around first aid and Cardio Pulmonary Resuscitation (CPR) training, health promotion and what to expect when you call an ambulance. This work has included attendance at events, school visits and work with community groups and has been undertaken by the PPI team, frontline staff, and volunteers from both the CEG and community first responders.
Over the next 6-months, the focus for engagement activities will be ‘how to be a good bystander’, things you can do as a member of the public to assist in an emergency, and engagement and education on what happens when you call 999 and how your call may be managed. The aim of this is to increase public awareness of the service and how we can all contribute to positive patient outcomes.
Patient and Family Stories
Our discovery interviews with patients or their families supplement our other feedback received by giving people the opportunity to share their story in their own words. These are filmed and are shown at public board meetings and discussed by the board. We have used them this year to support learning from complaints and serious incidents and find that hearing directly from the patient is a powerful learning tool. This year we have completed discovery interviews on areas such as end of life, staff attitude and behaviours, non-conveyance to hospital through working with the patient safety team, and delayed responses.
Links with HealthWatch and Patient Representative Groups
Our PPI team and our Community Engagement Group volunteers regularly attend a variety of meetings of patient representative groups including mental health groups, diabetes groups, young carers meetings and Healthwatch. We continue to expand our representation with other organisations and specialist groups across the region.
Raising concerns and Freedom to Speak Up
Within 2024/25, we recognised the opportunity to provide a more comprehensive independent and resilient Freedom to Speak Up process, and in August 2025, following consultation with the National Guardians Office, the Trust transitioned to an external provider, The Guardian Service.
The Guardian Service delivers comprehensive support to all EEAST personnel on a continuous basis—24 hours per day, 7 days per week, throughout the year, a facility we had previously not been able to provide to our staff. This service maintains complete confidentiality or anonymity, with guardians accommodating staff consultations through multiple channels: in-person meetings, Microsoft Teams conferences, or telephone communications to address any Freedom to Speak Up concerns.
Due to this change, we are, unfortunately, not able to provide a comparison for previous years and the following information relates to outcomes from 01 August 2024 to 31 March 2025. We will be able to provide a comparison in future years.
| Subject | Total number of concerns | Percentage (of total concerns) |
|---|---|---|
| Patient safety/quality | 4 | 2.44% |
| Worker safety or wellbeing | 11 | 6.71% |
| Bullying or harassment | 13 | 7.93% |
| Behaviour/relationships | 32 | 19.51% |
| Discrimination and inequality | 6 | 3.66% |
| Management issue | 29 | 17.68% |
| System and process | 68 | 41.46% |
| Other | 1 | 0.61% |
| Total | 164 |
During this period Trust staff raised 164 concerns via The Guardian Service, with the largest theme relating to system and process (41.46%), with behaviour and relationships accounting for 19.51% and management issue for 17.68%.
To date, 69/164 cases have been resolved either verbally or in writing and a further 15 staff (9.15%) have chosen not to pursue their concern. In 21 cases (12.80%), there has been no further contact from the member of staff following the concern being raised and the Service following this up.
At the time of this report there are currently 59 cases open and ongoing.
The Trust's two dedicated Guardians often visit stations and other locations. They maintain regular consultations with the Board to discuss prevalent concern themes, exemplary practices, and strategic recommendations.
In addition to the Freedom to Speak Up service, staff are also able to raise concerns to our People Services directorate in line with our policies and procedures, the outcomes of which are monitored and reported to our Trust Board through our Raising Concerns Forum.
We have recently applied to the Care Quality Commission for an existing condition relating to how we manage concerns to be lifted and, at the time of this report, are awaiting their decision.
Working with our local communities
We are supported by around 1,000 active and valued volunteers and other partners in a number of roles.
Community first responders
Our community first responders (CFRs) are volunteers who are trained by us to attend certain types of emergency calls in the area where they live or work. Their aim is to reach a potential life-threatening emergency in the first vital minutes before the ambulance crew arrives. Their role is to help stabilise the patient and provide the appropriate care until the more highly skilled ambulance crew arrives on scene to take over the treatment.
They also promote community partnerships and integrated working.
Volunteer car drivers
Working with our Non-Emergency Patient Transport Service, our volunteer car drivers are essential to help us provide an additional ambulance car service to our patients helping to take them to hospitals and other services.
Co-responders/ Collaborative Response
Military Co- responders Primarily composed of active military personnel and civil servants based at military bases, their role is to provide additional response capacity to EEAST by providing rapid response capabilities, thereby enhancing overall performance and patient care.
Fire and Rescue Service (FRS) partnership sees us working with six fire services under memorandum of understandings enabling them to respond for the Trust to a selection of calls. These include cardiac arrest response, immediately life-threatening calls, and bariatric assistance. They have also been instrumental in responding to our non-injury patients who have fallen. For more information regarding this please see page 36.
Emergency responder (ER) scheme. In March 2024, EEAST undertook an initial pilot to establish an emergency responder scheme based at our west Hertfordshire ambulance station. The aim of the scheme, comprised of volunteers from multi-disciplinary backgrounds including fire-fighters, police officers, and civil servants, is to provide an additional response resource within a sector that has previously seen prolonged C1 responses whilst developing and enhancing volunteer opportunities within EEAST. The scheme also incorporated a number of EEAST CFRs to aid onward volunteer progression and development. This scheme has since been expanded to include the addition of a second ER car in collaboration with the Beds and Herts Emergency Critical Care Scheme (BHECCS).
Achievements in 2024/25
- Safer recruitment processes for all volunteering roles.
- Provided specific additional training and continuous professional development (CPD) events.
- Expansion of FRS collaboration along with creation on dedicated team to support collaborative working.
- Secured three national awards for FRS collaboration work.
- Launch of new Emergency Responder scheme in collaboration with Beds and Herts Emergency Critical Care Scheme (BHECCS).
- Launch of our new Volunteer Management System.
- Roll out of Trust email address to volunteers to facilitate access to online learning platforms.
Looking forward
We have a number of activities and measures planned for 2024/25 including:
- Review of our volunteer governance structure which will include oversight of mandatory and statutory training compliance.
- Expansion of collaborative activity with FRS partners across the region to enhance co- responding model.
- Additional recruitment to be undertaken to support Military co- responder schemes along with the launch of a fifth team.
- Volunteers’ week – to be held at the beginning of June 2025.
- Expansion of lower acuity responses undertaken by both volunteers and FRS partners.
- Introduction and embedding of new volunteer roles.
For more information about how to become a volunteer, please go to our volunteering and volunteers page.
Commissioning for Quality and Innovation (CQuIN)
The CQuIN scheme is intended to deliver clinical quality improvements and drive transformational change and will impact on reducing inequalities in access to services, the experiences of using them and the outcomes achieved. Our CQuINs are agreed with our commissioners as part of our contract negotiations and have traditionally been a mix of nationally mandated and locally determined Quality and Service Delivery Improvement Programmes.
Since the Covid-19 pandemic CQUIN deliverables were largely suspended by NHS England which have not yet been re-instated
As such, there were no locally determined CQUINs in 2024/25 and the only national CQUIN for Ambulance Services related to the uptake of the flu vaccine, as there is each year in support of the protection against infectious illness. EEAST, achieved 33% for all directly employed staff which is considerably lower than achievements in previous years.
Although 39% of UEC operations staff did receive this, uptake was much lower among other staff groups.
Several lessons have been learned for the 2025/26 vaccination programme with four key improvement areas identified:
- Incentives – to encourage staff to be vaccinated.
- Vaccinator lead role – to ensure effective coordination of clinics, stock and vaccine fridges
- Bespoke software – to improve the process for appointments, reminders and to generate reports.
- Utilising welfare wagons – to improve accessibility for staff.
Poster displayed on our premises to encourage staff to receive vaccinations.

Quality success throughout the year
Pre-hospital stroke Video Triage (PVT)
Building on the successes seen in phase 1 which occurred in 2023, the South Integrated Stroke Delivery Network applied for funding for project continuation and was awarded a bid of £183,000 to expand the delivery of this service within phase 2.
Phase 3 funding was awarded in October 2024 with £192,673 to support the delivery of PVT globally within the region and to work towards embedding PVT as business as usual in the east of England.
PVT enables pre-hospital clinicians to connect with in-hospital stroke specialists via video call on their Trust issued iPad. The video triage is initiated on scene, allowing the ambulance and in-hospital clinicians to agree the correct pathway for the patient.
At the time of this report, 11 of the 15 stroke centres within our region have implemented PVT with a 12th currently being supported through the early stages of go-live.
Although usually resulting in a slightly longer time crews spend on scene, several positive outcomes have been determined from the trial to date, including;
- video triage delivers faster and more consistent times from hospital arrival to imaging
- more sensitive triage decisions are made when compared to the two most used pre-hospital stroke screening tools in the UK (FAST and BEFAST)) thus highlighting fewer missed stroke patients in the pre-hospital phase.
- Arrival at hospital to handover was reduced when compared to EEAST’s average.
Overcoming barriers Close partnership working with other UK ambulance service trusts identified that challenges associated with connectivity are on a national scale. In the east of England we felt that the inability to use PVT in some parts of the region leads to a health inequity – with many patients unable to access the early specialist input, triage, rapid imaging and expedited treatment that stroke video triage facilitates.
Discussions with Excelerate Technology regarding the impact of poor connectivity led to the commencement of a trial in mid and south Essex with five ambulances in the area being fitted with 4G long-term evolution (LTE) Optimisation Antenna to enable on-board Wi-Fi capability.
What our patients and staff say Part of the trial included a patient survey and feedback from our clinicians who had used this service. Results from the patient survey can be found within our patient feedback section on page 51. In relation to staff feedback, this has been mainly positive with over 75% of staff saying that they would like this to continue.
“Stroke is often a difficult prehospital assessment and is amazing to have expert assessment accessible. When the stroke diagnosis is obvious it can improve time to treatment with minimal effort so can't be a bad thing.” Feedback from a member of our staff who used this process
Cardiac Care
Following a Patient Safety Incident review into missed myocardial infarction, we introduced several initiatives in 2024/25 to improve cardiac care in the region.
- We have procured Glasgow software to go onto all of our Corpuls 12-lead ECG monitors which will provide automated ECG interpretation. This software has a high sensitivity for STEMI and will support our staff to recognise STEMI ECG changes. Rollout of the software will be completed by November 2025.
- We have also delivered a series of ECG training sessions, delivered by a subject matter expert at locations across the region. These have been available to all staff and have covered basics through to advanced ECG interpretation. More than 700 staff have attended these sessions to date.
- We have also commissioned 45 bespoke ECG training sessions for our clinical advice line colleagues, recognising the importance of their skills in ECG recognition, as they are the signposted source of advice for staff requiring ECG support.
Ultrasound supported decision making in urinary catheterisation
Our urgent care teams have developed their capabilities this year by introducing point of care ultrasound when undertaking primary and re-insertion of urinary catheters. The team has undertaken bespoke training in the utility of ultrasound prior to being signed off to use it in clinical practice. The ultrasound software allows for bladder volume calculation to be made pre and post catheterisation. Multiple patients have benefited from this development, often facilitating immediate relief of discomfort and allowing for community management, avoiding unnecessary hospital admissions.
Pneumofix device
We identified an opportunity for service development relating to the equipment provided for needle thoracocentesis. We were using intravenous cannulas, which were not specifically designed for this purpose, and therefore were not always successful in relieving pneumothoraces (when air leaks into the space between the lung and the chest wall, causing the lung to collapse).
In March 2024 we began to introduce the Pneumofix 8 device which is specifically designed for needle thoracocentesis (procedure used to relieve pressure in the chest cavity) in patients with a tension pneumothorax (severe and life-threatening condition where air builds up within the chest cavity (pleural space). This device is longer and more ridged in structure providing a more secure fitting and improving patient care for trauma patients. The devices are now available within all of our responding platforms, providing better care to patients with tension pneumothorax.
Advanced Practice Team urgent Care
Our advanced practice (AP) team continues to go from strength to strength completing their 30,000th patient contact in March 2025. The team continue to deliver excellent care, achieving around 75% non-conveyance overall which provides huge benefits to patients and the healthcare system, ensuring patients who are safe to do so, remain in the community, often with onward referral to system partners.
Most of our advanced practice clinicians continue to develop through their academic pathways with a number finishing MScs this year, as well as increasing the number of independent prescribers in the team this year to 36 .We have also increased the number of staff trained in the team to work within our emergency operations centre (EOC), supporting staff remotely with clinical advice, decision making support and community pathway access. We have also been able to accredit several of our AP team into Advanced Clinical Practitioners (ACPs), providing increased supervision capacity for our learners.
Our team have been involved in supporting the wider clinical workforce in a number of ways, including running wound closure courses. We have also been able to deliver development weeks for the team, in collaboration with NHSE and university partners.
Palliative End of Life Care medications
In 2024, advanced practice (AP) clinicians were authorised to administer Palliative End Of Life Care (PEOLC) medications following bespoke training designed and delivered in collaboration with EEAST and The Hospice of St Francis. Initially launched as a six-month trial, the initiative provided medication to 25 patients, ensuring they could remain at home in comfort.
Following the trial’s success, the programme has been fully implemented across the Trust and to date, 166 patients (live data capture) have received essential symptom management from APs, addressing pain, excessive secretions, breathlessness, nausea and vomiting, restlessness, and terminal agitation. A broad range of PEOLC medications have been administered to provide effective relief.
While many patients on a palliative care pathway should have anticipatory medications at home, this is not always the case. Thanks to this initiative, 98% of patients have been able to remain at home in a more comfortable environment, with additional specialist and community support referrals made when needed. This project has made a significant difference in ensuring that those at the end of life receive timely and compassionate care in their preferred setting. We are very proud of the team, who also won a Stars of EEAST award for Excellence in Patient Care Award for this initiative.
‘It has been immensely gratifying to be able to ease the final hours of patients and address their discomfort and fear, enabling them to die in their preferred place, often with their families around them. The families really appreciate the efforts of the ambulance service and are grateful that we can overcome the barriers to care that they have often been encountering’. - EEAST advanced paramedic
Locality Clinical Manager (LCM)
In 2024 we introduced a new clinical manager role to the organisation. The sector clinical lead team have designed and delivered a bespoke induction training package for this new role which includes; clinical supervision, cardiac arrest, trauma care, maternity training, performance under pressure, managing incidents, debriefing and welfare support to name a few.
The LCMs are now embedded into their localities, supporting with oversight of clinical supervision activities, professional update training as well as day to day support of our clinical workforce across various domains. We are already seeing the tangible benefit of having clinical leaders at a local level with lots of specific (continuous professional development) CPD provided based on the local need.
Training
In addition to our statutory and mandatory training for our clinicians, we also provide further in-depth learning, two examples of this are:
Maternity training
We have developed several training opportunities for our front-line staff in the past 12 months to support them in delivering effective care to obstetric and newborn life support calls. We have continued to deliver Practical Obstetric Multi-Professional Training (PROMPT) courses in partnership with education centres, for all registered healthcare professionals joining the Trust. We have also delivered a mini-PROMPT course to over 100 additional staff, covering the essentials in a day’s session.
We have been able to support 20 operational staff to complete a Newborn Resuscitation Course, run by the Resuscitation Council UK.
These staff will go on to cascade their training to peers throughout the coming year, several of whom will also be delivering the course as part of the national faculty.
We have also purchased several high fidelity premature/infant mannequins which are designed to increase the fidelity of simulation and allow for staff to be more familiar with gestation estimation, which has a critical influence on care delivery. We have also implemented a regional maternity pre-alert tool which has allowed us to standardise practice across the region and mitigate some of the risk associated with handing over of care relating to complex and often stressful clinical situations.
Trauma training
We identified that silver trauma (major trauma sustained by individuals aged 65 and older) constitutes a significant proportion of trauma patients within the east of England. These patients, who sustain significant injury through low energy mechanisms such as a fall from standing at home, are likely to have a significant injury burden. We were successful in applying for funding through the East of England Trauma Network to provide staff with the opportunity to access training by subject matter experts from Cambridge University Hospital. These days specifically focused on recognition, assessment and management of this patient group to help enhance patient care and ensure injuries are identified and appropriately managed. We also secured funding to provide similar training opportunities for staff relating to paediatric trauma care, which is another area of clinical practice where assessment and injury differentiation can be complex.
Quality Governance Committee Assurance
Strategic Goals
- Goal 2: Provide Outstanding Quality of Care and Performance
Strategy Overview Areas
- Clinical Strategy
- Research and Innovation Strategy
- Quality Improvement Strategy
- Quality Account Priorities
Strategic Risks and Risk Overview Areas
- SR2: Failure to achieve continuous quality improvements and high quality care
- Clinical and Patient Safety
- Safeguarding
- Infection, Prevention and Control
- Estates
- Medical Devices
- Medicines Management
Key Change Initiatives
- CQC Improvement Plan
- Medicines Management Programme
- QI Faculty Development
- PAS Oversight Framework
Key Performance Indicators
- SI number, harm and actions
- IPC audit compliance
- Safeguarding compliance
- PAS metrics
- Drug audits and incidents
- Complaint metrics
- Fire and first aid compliance
- Clinical Quality Indicators
Key Independent Assurance Mechanisms
- Regulatory inspection reports
- Internal audit reports
- Healthwatch opinion
- Independent reviews
- Benchmarking
Sub-Group Structure
Compliance and Risk Group
- Patient Safety Group
- Clinical Best Practice Group
- Medicines Management Group
- Safeguarding Group
- Infection Prevention and Control Group
- Patient Experience and Engagement Group
- Medical Devices Group
- External Provider Assurance Group
Statements from stakeholders
Statements from the Commissioners, HealthWatch and Overview and Scrutiny Committees
Suffolk and North East Essex
East of England Ambulance Service (EEAST) Annual Quality Account
Date: 16 May 2025
The Suffolk and North East Essex (SNEE) Integrated Care Board (ICB) confirm that EEAST have consulted and invited comment regarding the Annual Quality Account for 2024/2025. This has been submitted within the agreed timeframe and SNEE ICB are satisfied that the Quality Account provides appropriate assurance of the service.
SNEE ICB have reviewed the Quality Account and the information contained within the Quality Account is reflective of both the challenges and achievements within the organisation over the previous twelve month period.
SNEE ICB look forward to working with clinicians and managers from the service and with local service users to continue to improve services to ensure quality, safety, clinical effectiveness and a good service user experience is delivered across the organisation.
This Quality Account demonstrates the commitment of EEAST to provide a high quality service.
Lisa Nobes, Chief Nursing Officer Suffolk & North East Essex Integrated Care Board
Healthwatch Suffolk
Response to the East of England Ambulance Service NHS Trust Quality Account 2024/2025
Healthwatch Suffolk thank the Trust for the opportunity to comment on the Quality Account for 2024/25. We recognise this has been a period of extreme intensity for the Trust’s staff, clinicians and volunteers. As a Healthwatch, we are naturally also acutely aware of the heightened and at times sadly, unmet needs of the public, during these past 12 months. The number of 999 calls for 2024/25 was higher than in the previous year, at an average of over 28,300 calls a week. This equates to yet another challenging period for the Trust and its NHS partners.
Healthwatch Suffolk is the region’s local healthwatch representative for the East of England Ambulance Service NHS Trust (EEAST). We liaise directly with the Trust’s Suffolk based commissioners (Suffolk & North East Essex Integrated Care Board), and we are also informally responsible for coordinating regionwide healthwatch engagement with EEAST. This does of course only take place successfully because of the proactive support of the other local healthwatch in the east.
People in Suffolk rated their experiences of the Trust at about 31/2 stars out of 5 on average, during 2024-25. Half of the comments received were entirely positive in sentiment, whilst just over 1 in 6 were entirely negative. Themes centred around Staff and Waiting. Six of our region’s local healthwatch have kindly shared their Statements with us, helping to identify common themes, observations and suggestions. Listed in alphabetical order, they are Healthwatch Cambridgeshire & Peterborough, Healthwatch Central Bedfordshire, Healthwatch Essex, Healthwatch Hertfordshire, Healthwatch Norfolk, and Healthwatch Southend. They have each studied EEAST’s draft Quality Account and offered reasoned and constructive feedback. Their individual Statements are included as Appendices to this Statement.
Themes raised include references to:
- Welcoming the Trust’s continued commitment to the importance of patient experience in bringing about quality improvement and safety e.g. twelve separate co-produced surveys (noted by all seven local healthwatch).
- Welcoming an approach to involving young people and for improving service satisfaction for young people. All local healthwatch expressing this sentiment offer EEAST their help in achieving such ambitions, because of their own work with and for young people (noted by six local healthwatch).
- Noted the several Care Quality Commission concerns raised over the past 3 years, with a recognition from some that improvement action plans are gradually making progress (noted by six local healthwatch).
- Welcoming the Trust’s wish to expand and diversify its reach demographically, when it comes to engaging the public. The important contributions of the Community Engagement Group are noted. Each local healthwatch offers the Trust assistance in helping to achieve such ambitions (noted by five local healthwatch).
- Commending the collaborative approaches made by EEAST in working with Hospitals regarding handovers, and in some parts of the region, the Fire & Rescue Service regarding falls (noted by five local healthwatch).
- A view that EEAST would achieve more impact and perform better by meaningfully engaging with its local healthwatch organisations (noted by four local healthwatch).
- C2 call concerns and handover delays (noted by four local healthwatch).
- Welcoming the achievements of the Unscheduled Care Co-ordination Hubs (noted by four local healthwatch).
- As has been raised in previous years, concerns about the lack of Quality Account data and performance not being broken down according to either
- local healthwatch areas (coterminous with local authority boundaries) or (ii) integrated care system boundaries (noted by four local healthwatch). As an example, the planned closure of the Bedford Call Centre in 2025, not referenced in the Quality Account, is understandably of particular concern to Healthwatch Central Bedfordshire. Please note that EEAST had committed to arranging a workshop with local heathwatch for September 2024, with the intention of exploring how best to make such changes. Sadly, this event never occurred.
- Welcoming initiatives to address Admisison Avoidance (noted by four local healthwatch).
- Noting that complaints have reduced in number/percentage (noted by three local healthwatch).
- Welcoming employment cultural workplace improvements, the Freedom to Speak Up Service and results of the national Staff Survey (noted by three local healthwatch).
- Welcoming the Trust’s growing response to the public’s needs on accessibility, in for example its approach to surveying the public (noted by three local healthwatch).
- Welcoming the work around Quality Action Reviews and Learning from Deaths (noted by three local healthwatch).
Inaugural co-production training was provided by Healthwatch Suffolk through several workshops in 2021, eventually also leading to the creation of what is likely to remain a unique ambulance trust Patient & Public Involvement Strategy ‘on a page’ in 2021/22. We therefore welcome all the references to co-production, and the power of bringing lived experience into decision making at the Trust. Perhaps a healthwatch led evaluation with staff and volunteers involved in such co-production initiatives, might underpin how far the Trust has come these past 3- 4 years?
We welcome the positive news that the unscheduled care co-ordination hub in Norfolk and Waveney has diverted 62% of their calls from the stack since its launch in September 2023, thus avoiding unnecessary ambulance responses and proving system efficiency. Sadly, the single biggest contributor to C2 response times remains hospital handover delays.
Other positive highlights we acknowledge include:
- The launch of the new 24 hour & 365 day a year Freedom to Speak Up Service for staff will be appreciated by the Trust’s staff. Only 6% of CQC 2022 inspection actions remain outstanding.
- The Trust officially opened its first net zero ambulance hub in Bury St Edmunds. Staff also have access to a quiet room for their wellbeing, a multi-faith room, nursing room, gym and outside wellbeing space for rest and relaxation.
- Leadership Development Framework
- The Trust launched urgent and emergency care hubs in ‘all’ counties, in partnership with the ICBs.
- The Trust benefits from more than 1,000 dedicated volunteers, such as community first and military co-responders, volunteer car drivers, BASICS doctors, chaplains, and its Community Engagement Group. We look forward to learning more about the Emergency Responder Scheme pilot in West Hertfordshire.
The current ‘quality position’ of the Trust shows improvements in ambulance responses against categories 3 and 4, alongside increased advance practice in urgent care, through the expansion of Unscheduled Care Hubs across all areas of the Trust. We would like to know more about why the introduction of artificial intelligence within Emergency Operational Centres is already considered a success. Has there been an evaluation of the use of such technology?
We note that the CQC has submitted a Section 64 notification that requests further improvements to be made, particularly to Category 2 responses. The Trust had been inspected (unannounced) in November 2024, with a focus on Urgent and Emergency Care (UEC) and Emergency Operations Centres (EOC).
This led to a Section 29a Warning Notice issued in January 2025 by the CQC, which requires the Trust to focus on improving mandated training compliance, medicine management investigations, call pick up performance and looking to engage better with the staff and continue to work on the cultural improvements. A CQC Section 64 letter, also issued in January 2025, requires the Trust to address matters concerning regulated activities, good governance, and safe care & treatment.
We acknowledge positive news such as the fact that all mandated training is now above the required target of 85% for all staff groups and competencies. 95% of the ‘must dos’ and ‘should dos’ from the 2022 CQC report have been closed.
For the fifth year running, the Trust has exceeded the national ambulance average for its quality indicators; heart attack, stroke, and cardiac arrest survival, to discharge for those patients where the arrest was bystander witnessed, and the initial heart rhythm was ventricular fibrillation or ventricular tachycardia.
As a local healthwatch we would like to bring to the Trust’s notice that we are at times invited to contribute to Rapid Quality Reviews. We note that such a Review had taken place, with a membership that includes “Suffolk and North East Essex Integrated Care Board (ICB)”. We welcome the choice of strategic priorities:
- Priority 1 patient safety; of note, “to further embed the Learning from Deaths process at EEAST” and “enhance the way in which we share learning from incidents, complaints and claims.”
- Priority 2 clinical effectiveness; of note “pain management”.
- Priority 3 patient experience; of note “expand the analysis and reporting from the patient surveys program to include reporting of experiences by different demographic groups”, “ensure that education about changing services and clinical model is part of patient engagement”, and “expand CEG membership to include 16/17-year-old members to represent younger patients’ views.”
In reference to Priority 3, please note that the local healthwatch operating across the Trust’s geographical patch, are able to:
- enhance any ambitions for identifying “ways to improve patient experience for specific groups”,
- Help patients to have a better “understanding of the range of services that the ambulance service now provides”, and
- Help reach the Trust’s new target (16-24) population age group, thus increasing the Trust’s “understanding of their experiences and expectations to allow learning and improvement”.
There is an understandable mixed bag of performance related news, considering the significant pressures on our national and local NHS services.
The Trust has not meet national standards, except for Category 1 calls. That said, “March 2025 saw the best response times for the year for all categories”.
The largely rural aspect of our region continues to contribute towards the Trust’s ability to try and meet the national standard of 15 minutes for the handover of a patient to the receiving hospital. Additional deep winter pressures led to such handover times to average over 50 minutes in January 2025.
We welcome the successful use of collaborative Handover Units with local hospitals, facilitating quicker patient transfers e.g. “for instance, at Southend Hospital, a 12-patient capacity unit was established to expedite handovers, allowing ambulance crews to return to service more promptly. This initiative aims to enhance patient care by ensuring timely medical attention and reducing ambulance turnaround times.”
We would however seek some level of assurance (more detail about the management of patient safety risk) in the Trust’s adoption of its “Handover 45(HO45) policy in November 2024” i.e. “if a patient handover is not completed within 45 minutes, ambulance crews may leave the patient in a designated area within the ED, provided the patient is clinically stable.”
We note the excellent news concerning alternative care pathways such as the Hear and Treat (H&T) service, “in May 2024 8.7% of patients were treated through this service, in December 2024 this number had risen to 12%, meaning that more ambulances were available for our sickest patients.”
Other welcome news include:
- All Integrated Care Systems within the east of England has a functioning Unscheduled Care Coordination Hub (UCCH). An EEAST clinician is now co- located as a member of the multi-disciplinary team within each ICS, every day.
- STEMI (heart attack care) care bundle is achieving an average of 93.2% for the year to date, with EEAST the second highest performing Trust for this care bundle ,achieving 15.0% above the national average.
- Patient safety (next steps) aim over the next 12 months to train 85% of band 7 managers in after action reviews, and this has been set as a priority for 2025/26.
- In terms of safe discharge of patients left on scene (clinical effectiveness), only one serious patient safety event relating to the non-conveyance of a patient has been identified in-year.
- During 2024/25, EEAST participated in 100% of all required national clinical audits.
The Trust’s collaboration with Fire and Rescue Services, concerning falls in older people non-conveyed, now has a Community Wellbeing Officer operating in Bedfordshire, Cambridgeshire and Essex. Are there plans to introduce such a role in other parts of the region e.g. Suffolk, Norfolk?
We acknowledge the twelve bespoke patient experience survey projects that have been undertaken during 2024/25. It is good to note that such surveys are available in a range of formats, including a co-produced Easy Read version.
There has been a focus on admission avoidance schemes and patients who had received assessment/treatment within the home setting. Overall, 97.0% of patients who were cared for through this process have reported satisfaction.
The Trust is continuously learning, which is positive, and now recognises that in “breaking down data for demographical analysis, it became apparent that most survey feedback comes from older, white British patients” and not reflective “of the communities we serve”. Once again, the local healthwatch operating across EEAST’s patch can help in accessing a far wider population and their experiences of ambulance services.
Likewise, local healthwatch can help by engaging the public on initiatives such as the development of the next patient and public involvement strategy. We note that “many patients and members of the public felt unable to provide critique or constructive input into what the ambulance service should do over the next 5 years as they felt that they did not understand how the service worked beyond a blue light response”. Such engagement and dialogue with the public, on behalf of NHS and other public health and care bodies, is one reason why healthwatch was included in the Health & Car Act (revised 2022). It is a missed opportunity when not utilised.
Several local healthwatch organisations have expressed an interest in hosting one of the Trust’s Patient Engagement Forums once a year; Central Bedfordshire, Norfolk and Suffolk, amongst those who are interested in doing so. The Patient Safety Incidents charts (on page 46) need to be bigger and have their multi-themed/coloured bars numbered, per theme. The two charts in question centre around “the number of delay incidents vs the total number of patient safety incidents” and “the number of patient safety incidents reported versus our activity during the year”. The two charts, as they are now in draft form, are very unclear about what they are conveying to the person reading them.
The table featuring the Duty of Candour (DoC) data, comparing 2024/25 with the 3 preceding years, suggests that whilst there has been a sharp drop in the number of cases, which is welcomed, the corresponding “average timeframe for DoC to occur (working days)” has increased from a low 4.0 in 2022/23, to what was 7.0 in 2024/25.
As in all previous years, compliments far outweigh the number of complaints received by the Trust, and “consistently increased year on year for the last 3 years”, which is excellent news.
In terms of complaints, “the biggest theme from complaints and concerns was delay, with most of those complaints (62%) being related to The Patient Transport Service (PTS) rather than Urgent and Emergency Care (UEC) service or our Emergency Operations Centres (EOC).” The next biggest themes were “transport and driving”, “attitude which is largely related to the Trust’s UEC service” and “clinical assessment and treatment”. We note the positive news that “delay complaints were reduced by 30% compared to 2023-2024”.
We also note that in 2024/2025, the Trust was not notified of any cases which had been referred to the Parliamentary and Health Services Ombudsman (PHSO) by complainants.
The Patient and Public Involvement team and Community Engagement Group volunteers regularly attend a variety of meetings of patient representative groups including mental health groups, diabetes groups, young carers meetings and Healthwatch. In reference to EEAST’s introduction of ‘trauma training’ for staff, “specifically focused on recognition, assessment and management of this patient group to help enhance patient care and ensure injuries are identified and appropriately managed”, please note and liaise with Healthwatch Essex on their now national Trauma Card initiative.
Overall, the Trust has made improvements, considering the challenges the Trust and its partners have faced during 2024/25, as described in the Quality Account. We are appreciative of your continued efforts and in your engagement of the public.
Andy Yacoub Chief Executive
Wendy Herber Independent Chair
HealthWatch Bedford
East of England Ambulance Service – Quality Account 2024/25
Healthwatch Bedford Borough (HBB) thanks the trust for the opportunity to respond to the quality account for 2024/25. The document offers a clear indication of how the trust work to achieve progress.
The progress which the trust has made in terms of meeting its regulators’ requirements is welcomed, following what has, no doubt, been a challenging year for the workforce locally following the November 2024 EOC inspection and internal consultation over estates.
Patient Experience The number of ways in which feedback has been used to improve service delivery is welcomed and we note that you have continued to undertake a patient survey programme to ensure views are obtained from patients who have accessed the service. However, HBB feels that there’s considerably more work to be done in bringing engagement out into the communities across Bedford Borough in settings where patients and local people feel comfortable in. Your lack of regular presence at community events and groups as well as attendance in professional meetings is noted by patients and stakeholders. This is an area that requires operational investment.
National response times and targets Whilst you did not meet respective metrics in some areas, we acknowledge the sheer volume of 999 emergency calls that the trust has coming in every day. Also noting that the inability to meet respective metrics was often through circumstances out of your control including winter pressures on the NHS. We remain disappointed that the quality account does not allow us to examine and celebrate the variations at a local level, as opposed to trust-wide reporting only.
We are pleased to see the reduction in a considerable number of response time categories from 2023/24. The trust should be congratulated on your ACQI STEMI care bundle compliance levels. It is encouraging to see that the trust is performing well above the national average of 76.8% in this area with 93% compliance. This is a testament to the work that has gone into this area over the past few years.
Patient safety and learning outcomes In relation to the shared judgement reviews under the Learning from Deaths programme and progress achieved against the trust’s target of achieving a minimum of 40 reviews per quarter, we are encouraged to see that not only did you meet your 160 reviews per annum total, but you achieved a year-end total of 400 completed reviews. This clearly demonstrates the trust’s willingness to learn.
Staff wellbeing We are pleased to read of the implementation of the trust’s ‘Time for Me’ wellbeing platform in May 2024. The early intervention element will prove itself invaluable when measuring risk factors. It’s use, in conjunction with wellbeing rooms for staff is encouraging.
Achievements of FRS Falls Collaboration HBB commends the trust on the success you have achieved thus far with blue light partners on the CWO model. This essential service provision clearly demonstrates clinical and collaborative success. The high percentage of cases closed without an ambulance attendance underlines the efficiency of the CWO team in attending lower acuity calls. This will also provide comfort for vulnerable patients, and we look forward to seeing further celebration of this programme’s success.
Healthwatch Bedford Borough looks forward to greater opportunities to work with the trust over the next few years.
Emma L. Freda, CEO
Healthwatch Cambridgeshire and Peterborough
East of England Ambulance Service (EEAST) Quality Account Statement 2024/2025
Healthwatch Cambridgeshire and Peterborough commends the East of England Ambulance Service NHS Trust (EEAST) for its commitment to prioritising patient experience as a key component of its quality improvement work. As part of the East of England Healthwatch Network, we know that consistently listening to patients and learning from their experiences is fundamental to delivering safe, compassionate, and responsive care across our region.
We welcome the Trust’s emphasis on expanding its patient experience programme, especially efforts to collect and analyse feedback from different demographic groups. This approach reflects our own priorities as a regional network, where we are working together to ensure that services are informed by the views of people from diverse communities, including those who are often underrepresented or face barriers to accessing care.
We particularly acknowledge and support the Trust’s decision to prioritise improving care for young people. The finding that a significant proportion of patient complaints originate from younger service users aligns with what we are hearing locally. Many young people, especially those aged 16 to 24, have shared with us that they often feel misunderstood or overlooked. Recognising these concerns as a formal priority is an important step toward building trust and delivering more age-appropriate, respectful, and inclusive care.
The Trust’s plan to include young people in its Community Engagement Group and to create safer processes for involving 16–17 year olds volunteers is a particularly welcome development. We believe that when services make space for young voices, not just as patients, but as active partners in service design and improvement, it can lead to powerful change. We look forward to supporting this ambition and sharing insight from our ongoing engagement with young people across the region.
As we look ahead, we encourage EEAST to continue building strong, transparent relationships with Healthwatch partners across the East of England. We also support the Trust’s work to embed learning from complaints, incidents, and patient feedback at every level of the organisation.
Yours faithfully, Jess Slater, Chief Executive, Healthwatch Cambridgeshire and Peterborough
Healthwatch Central Bedfordshire
EEAST: Annual Quality Account 2024-25
Last year Healthwatch Central Bedfordshire commented that the Quality Account lacked specific geographical/demographic details that might assist us put the report into our local context, our ‘lived’ experiences of your service provision. We note that other organisations made similar comments – It is disappointing to see that this years Quality Account still lacks that breakdown, and that information and data is generic covering the whole of the Trusts (geographic) area of responsibility. For example – what are the response times in Central Bedfordshire? How many Serious Incidents occurred in Central Bedfordshire? And this is pertinent because whilst reviewing this QA we saw in our local newspaper the plans to close the Bedford call centre, of which no mention within your report.
As ever we note the purpose of the Quality Account is set against the framework of the three overlapping key themes of patient safety, clinical effectiveness and patient experience, which each and together define ‘quality of care’.
And we can see from the Chief Paramedics report that he feels that the Trust has strived to continue to make improvements within both the quality and safety portfolio as well as in operational performance, for example for the fifth year running, you exceeded the national ambulance average for quality indicators; heart attack, stroke, and cardiac arrest survival. And we note that they you have accepted the feedback from the CQC that further improvements are still required and are actively addressing these.
We can see that following an unannounced visit the Trust expects a ‘Well-Led’ assessment from CQC. But we also are concerned that following on from 2022’s findings some of the areas highlighted in the 2022 inspection report were again found to be a cause of concern and we trust that these are receiving urgent attention.
That said, initiatives such as the ‘Clever Together’ campaign and ‘After Action Reviews’ are welcomed and we support the 2025/26 Priorities (P’s18-21) and the Patient and Public Involvement (PPI) Strategy (P39). Healthwatch Central Bedfordshire can quite see how Young Healthwatch might assist in the coming year, especially within your CEG (P59). We also commend the work done via the Guardian Service (P60-1).
Your aim for 2024/25 was to ensure that patient engagement and feedback was part of EEAST’s ongoing strategy with evidence of the patients’ voice throughout and you have supplied evidence of that throughout the document.
Operationally – it is as we have said, difficult to assess local performance based on generic figures and whilst we quite understand the numerous challenges that the Trust faces, for example meeting response times, and so perhaps the question to be asked is, are these realistic ‘targets’, when for example C2 and C3 response times are exceeded by such great margins (P23)? We liked the section on Admission Avoidance (P58) and support all that might be done in relation to that.
We are also encouraged by the ‘lessons learned’ your successes, as described from page 65 onwards.
There is a lot of information within this Quality Account and it is clear that the Trust is being open and transparent by highlighting many of the issues that it faces and its own results. However, it appears that the trajectory is ‘upwards’, with, in challenging times, progress being made in both quality of care and staff experiences in the work place. Thank you for giving us time to consider this report.
Diana Blackmun, Chief Executive Officer, Healthwatch Central Bedfordshire
Healthwatch Essex
Response to EEAST’s Quality Account 2024-25 from Healthwatch Essex
Healthwatch Essex is an independent organisation that works to provide a voice for the people of Essex in helping to shape and improve local health and social care. We believe that health and social care organisations should use people’s lived experience to improve services.
Understanding what it is like for the patient, the service user and the carer to access services should be at the heart of transforming the NHS and social care as it meets the challenges ahead of it.
We recognise that quality accounts are an important way for local NHS services to report on their performance by measuring patient safety, the effectiveness of treatments that patients receive and patient experience of care. They present a useful opportunity for Healthwatch to provide a critical but constructive, perspective on the quality of services, and we will comment where we believe we have evidence – grounded in people’s voice and lived experience – that is relevant to the quality of services delivered by East of England Ambulance Service NHS Trust (EEAST).
We offer the following comments on the EEAST Quality Account:
- It is disappointing to see areas of concern flagged by the CQC with regards to mandated training compliance, medicine management investigations, call pick up performance and staff engagement/cultural improvements, but we note the efforts made already to address these concerns.
- It is good to see a focus on staff safety and wellbeing through the introduction of the Freedom to Speak Up service and see the already demonstrated improvement in the staff survey. It is important to embed clinical supervision as a priority.
- We are pleased to see the strong commitment to patient engagement throughout the report, as we know that listening to patient feedback can make many improvements to services. We welcome the focus on increasing the engagement with younger people and ensuring the diversity of demographic groups engaged with. We appreciate the need to educate the public on your services to increase meaningful feedback.
- It is positive to see innovation, research and collaboration initiatives that will improve patient experience. In particular it is good to see new initiatives around hospital handover and reducing waiting times, as this remains to be an issue we hear regularly hear about. Collaboration initiatives with other emergency services are positive for enabling a joined-up approach.
Listening to the voice and lived experience of patients, service users, carers, and the wider community, is a vital component of providing good quality care and by working hard to evidence that lived experience we hope we can continue to support the work of EEAST.
Samantha Glover, Chief Executive Officer, Healthwatch Essex April 2025
Healthwatch Hertfordshire
Response to the East of England Ambulance Service NHS Trust (EEAST) Quality Account 2024/2025
Healthwatch Hertfordshire is pleased to provide a response to the EEAST Quality Account 2024/25.
It has been a challenging year for the Trust, and we recognize the hard work and commitment of staff to deliver against the CQC required actions to make quality and performance improvements together with cultural change, accepting that there is more to do. We welcome seeing the significant improvement of C3 and C4 response times in the latest period. However C2 performance in Hertfordshire is well below the required standard with handover delays also a cause for concern, leading to an increase in patient safety alerts. These areas will need continued focus to deliver safe and effective patient care.
Of particular concern for Hertfordshire is the workforce situation. Whilst we acknowledge that a number of initiatives have been trialled to address the problems, a more sustainable solution is needed.
It's good to see examples of system partnership working such as the Unscheduled Care Co-ordination Hubs that in Hertfordshire links up with Hertfordshire Community NHS Trust to reduce unnecessary hospital admissions and provides more immediate personalised care. The falls project with Fire and Rescue Services in some areas also shows a collaborative approach to improving patient care for vulnerable people.
We welcome the overall decline in complaints but note that issues with 'attitude' themes are still coming through the complaints process. Clear and empathetic communication is a key component of a positive experience of care.
The emphasis on culture shift is recognized as central to EEAST’s transformational plans and we welcome the introduction of Freedom to Speak Up champions and other initiatives to enhance staff support and empowerment.
Mandatory training compliance appears to be on an improving trajectory and this will need vigilance and focus to maintain and surpass this key indicator in order to provide a high quality service.
We welcome engaging patients and the public in raising awareness of the Trust’s work but would encourage regular conversation in shaping future work programmes and projects. In particular we welcome the focus on Children and Young People, as they are an underrepresented group, and the actions being put in place to hear their voices to help shape services. We will be exploring key issues within health and social care for Children, Young People and Families in the coming year and would be very happy to collaborate and share insights from this work with EEAST.
We note the action ‘to enhance analysis and reporting by demographic groups to better understand diverse patient experiences, whilst proactively engaging with seldom heard groups.’ Improving the collection and recording of patient ethnicity data to better capture the health outcomes of Black and Asian patients was one of the recommendations in our Making Local Healthcare Equal report. We look forward to seeing how EEAST proactively encourages people to provide demographic information and how they use this data to understand the communities they serve so that services can then be tailored to meet the differing needs of the population.
It’s good to see priority being given to coproduction of themed surveys with patients by experience to review delivered services, and especially good to see investment in accessibility through easy read and BSL videos. Our research has shown the importance of the consistent use of accessible information and reasonable adjustments to improve patient safety and experience.
We look forward to seeing the next stage of the Trust’s co-production and patient engagement initiatives to support service design, quality improvement and evaluation and how EEAST ensures people are not digitally excluded in next year’s Quality Account. The work of local Healthwatch to connect patient voice and experience could be valuable to EEAST in these changing times and we would welcome closer collaboration between EEAST and local Healthwatch overall.
We look forward to working more closely with EEAST in the coming year to ensure patient experience is central to EEAST’s development, including participating in the recruitment of key senior roles within the organisation.
Neil Tester, Chair Healthwatch Hertfordshire
Healthwatch Norfolk
Review of East of England Ambulance Service NHS Trust Quality Account 2024/25
Thank you for giving Healthwatch Norfolk (HWN) the opportunity to provide comments on the draft East of England Ambulance Service NHS Trust (EEAST) Quality Account for 2024-2025.
It has been another challenging year for the Trust with an increase in emergency contacts from the public since 2023/24 and in the context of increasing pressures on health and care system as a whole.
We note the recent notification from the Care Quality Commission (CQC) requiring further improvements to be made, particularly to Category 2 (C2) ambulance responses. We also note that EEAST is awaiting the draft report from the CQC’s inspection last November of Urgent and Emergency Care and Emergency Operations Centres, and that the Trust is anticipating recommendations which result in a new improvement plan.
In relation to C2 ambulance responses, we are pleased to see the collaborative working by the Trust with other parts of the health and care system. For example, the unscheduled care co-ordination hub in Norfolk and Waveney, which has made a significant contribution to avoiding unnecessary ambulances responses by ensuring alternative care pathways are available.
We recognise that delays in hospital handover make a contribution to C2 response times and note that, with the support of commissioners and acute Trusts, EEAST has led an initiative to facilitate quicker hospital handovers, which is making a positive impact in terms of reducing avoidable harm.
The Trust has continued to work hard with system partners to address the requirements of the CQC inspection in 2022 and 95% of the actions have now been closed, with the remaining actions relating to C2 response times, workforce development and organisational culture.
Quality Priorities for coming year In terms of patient safety, we are pleased to see the ongoing focus on the Trust as a learning organisation, with priorities around learning from deaths, incidents, complaints and claims, together with efforts to improve the quality of the learning and to enable shared learning across the organisation.
Under clinical effectiveness, we note that a priority has been identified on improving the documentation of pain scoring, which helps determine how effective any actions taken or treatment provided has impacted on the patient’s condition. We also note the use of new technology in several priorities, including piloting the use AI to reduce ‘on scene’ times and therefore ‘job cycle’ times which, in turn, impact on the Trust’s ability to respond to Category 2 patients in a timely manner. It will be interesting to see the outcome. Priorities around patient experience build on previous years’ improvement work, with plans to expand the analysis and reporting from the annual patient surveys programme to include reporting of experiences by different demographic groups and obtain feedback from those seldom heard. We also note the priorities around increasing public knowledge and understanding of the Trust’s services to enable more meaningful patient feedback, and increasing engagement with 16-24 year olds. If Healthwatch Norfolk can be of any assistance with any of these developments then please do get in touch.
Performance against quality priorities for previous year We note that the Trust has maintained its ambulance care quality indicators and has achieved some improvement to ambulance response times (categories 2, 3 and 4). Response times do, however, fall short of the national standards and in January 2025 the Trust received notification from the CQC requiring further improvements to be made to C2 responses.
The number of service provision hours lost is identified as a key factor affecting C2 ambulance service performance and the Account outlines a number of strategies that the Trust has in place for addressing this, including the ‘handover 45’ initiative to help address delays in handing patients over at hospitals and the Unscheduled Care Coordination Hubs with each Integrated Care System across the east of England.
We note that, following the CQC’s inspection in November 2024, the Trust also received a formal Warning Notice relating to some areas originally highlighted in 2022, including concerns regarding call ‘pick-up’ time and the number of staff within the emergency operations centres (EOCs). The Quality Account outlines how the Trust continues to develop its Clinical Assessment Service to enable patients to be treated correctly and we note that an increasing number of patients are being treated through the ‘Hear and Treat’ service.
We are pleased to see that progress is being made with embedding the Learning from Deaths programme, which continues as a priority for 2025/26. The Patient Safety Incident Response Framework is now well embedded in the organisation and we note that the process, which includes quality After Action Reviews, will continue to be used to inform learning with two further priorities set for 2025/26. In terms of patient experience and feedback, we note that complaints arose from 0.05% of the Trust’s contacts with patients, an improvement of 0.1% on last year, and that the number of re-opened complaints remains very low (1.2% of all complaints), indicating that the responses have addressed and/or resolved the questions and concerns.
It is interesting to see that during 2024-2025 a range of bespoke surveys were introduced with a focus on admission avoidance schemes and patients who had received assessment and treatment within the home setting, with an overall, 97.0% of patients reporting satisfaction and expressing support for the initiatives.
The Trust’s Community Engagement Group is clearly making progress in representing the patient voice, for example, through having a regular place and active role in Trust board meetings, working with the Patient and Public Involvement Team on ways to increase engagement, assisting with public engagement events, and contributing to the development of the Trust’s 2025-30 strategy. We note that for 2025/26 the focus is on diversifying the Group and encouraging younger engagement.
Accessibility EEAST’s Quality Account is clear, readable and available in other formats and languages. As such it is a valuable source of information to the public about the Trust’s priorities for improvement, what action is being taken, what progress is being made and what the next steps are. It would be helpful to know how the Quality Account is promoted to patients, staff, and wider stakeholders, once published on the Trust’s website.
Conclusion HWN recognises the ongoing efforts being made by the Trust - its staff, volunteers, and its leadership – to improve the quality of care provided. We are happy to assist EEAST in any way we can in ensuring the views of patients, their families and carers are taken into account as the Trust works to deliver the improvements needed.
Alex Stewart, Chief Executive, Healthwatch Norfolk
Healthwatch Southend
Response to the East of England Ambulance Service NHS Trust Quality Account 2024/2025
Healthwatch Southend recognises the important work which the Trust has undertaken to improve the experience and outcomes for people in the East of England. We appreciate the efforts taken to hear from service users and the way in which real life examples are used within the document to demonstrate learning.
However, we are disappointed by the recent Notices imposed on the Trust by the Care Quality Commission. As the Trust notes, some of these repeat concerns identified in 2022. We look forward to the Trust acting quickly to remedy the shortcomings and to providing accessible updates to local people about the progress being made.
In responding to previous Quality Accounts, we have asked for more monitoring data to be made available at a more granular level. Whilst many metrics are positive, it is difficult for an organisation like Healthwatch Southend to monitor whether its local residents receive a better or worse services than other parts of the East of England. We would call for an assurance that this will be addressed in 2025/6.
Yours sincerely
Owen Richards, Chief Officer
Suffolk County Council - Suffolk Health Scrutiny Committee
As has been the case in previous years, the Suffolk Health Scrutiny Committee does not intend to comment individually on NHS Quality Accounts for 2024-25. This should in no way be taken as a negative response. The Committee acknowledges the ongoing engagement and contributions made by the NHS to the work of the Committee and wishes to place on record our thanks for everything being done to maintain NHS services for the people of Suffolk.
County Councillor Jessica Fleming, Chairman of the Suffolk Health Scrutiny Committee
Glossary
| Term | Acronym | Definition |
|---|---|---|
| 90th centile | The value of a variable such that 90% of the relevant data is below that value. | |
| Accident and emergency | A&E | A medical treatment facility specialising in acute care of patients who present without prior appointment, either by their own means or by ambulance. The emergency department is usually found in a hospital or other primary care centre. |
| Advanced Practitioner | AP | A healthcare profession with extended qualifications and scopes of practice. |
| After Action Review | AAR | A method of evaluation that is used when outcomes of an activity or event, have been particularly successful or unsuccessful to capture learning. |
| Ambulance (clinical) quality indicators | ACQIs | A set of national measures to benchmark clinical quality against eleven indicators to improve quality and safety of patient care. |
| Artificial Intelligence | AI | The theory and development of computer systems able to perform tasks normally requiring human intelligence. |
| Association of Ambulance Chief Executives | AACE | A central organisation that supports, coordinates and implements nationally agreed policy. |
| Blood pressure | BP | The pressure exerted by circulating blood upon the walls of blood vessels. One of the principal vital signs. |
| British Association for Immediate Care | BASICS | A charitable organisation who works in partnership with EEAST |
| Cardiopulmonary resuscitation | CPR | An emergency procedure, performed in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person in cardiac arrest. |
| Care Quality Commission | CQC | The independent watchdog for healthcare in England. It assesses and reports on the quality and safety of services provided by the NHS and the independent healthcare sector, and works to improve services for patients and the public. |
| Category 1 | Cat 1 | National response time standard for 999 immediately life-threatening injuries and illnesses. |
| Category 1T | Cat 1T | National response time standard for 999 immediately life-threatening injuries and illnesses where the patient is transported. |
| Category 2 | Cat 2 | National response time standard for 999 emergency calls. |
| Category 3 | Cat 3 | National response time standard for urgent calls and in some instances where patients may be treated in-situ (e.g., their own home) or referred to a different pathway of care. |
| Category 4 | Cat 4T | National response time standard for less urgent calls. In some instances, patients may be given advice over the phone or referred to another service such as a GP or pharmacist. |
| Chief Executive Officer | CEO | The position of the most senior officer, executive, or administrator in charge of managing an organisation. |
| Clever Together | A company that helps organisations and progressive leaders improve performance and outcomes by incorporating evidence, expertise, and lived experiences into decision-making. | |
| Clinical Assessment Service | CAS | An EEAST service to provide triage to patients who have accessed the 999 service. |
| Clinical Audit | - | A process for measuring the level of care given against a set of standards to drive improvement. |
| Commissioning | - | The processes which local authorities and clinical commissioning groups undertake to make sure that services funded by them meet the needs of the patient. |
| Commissioning for Quality and Innovation programme | CQuIN | The incorporation of quality metrics within quality and innovation three-year contracts. Full reimbursement of activity is made upon delivery of quality initiatives. |
| Community Engagement Group | CEG | A group within EEAST in place to ensure that views of patients and their representatives can be used to improve our services. |
| Community first responders | CFR | Teams of volunteers who are trained by the ambulance service to a nationally recognised level and provide lifesaving treatment to people in their communities. |
| Cyber Assessment Framework | CAF | A systematic and comprehensive approach to assessing the management of cyber risks to essential functions of organisations. |
| Data Protection Act | DPA | United Kingdom Act of Parliament which updates data protection laws in the UK. |
| Data Security Protection Toolkit | DSPT | An online system which allows NHS organisations and partners to assess themselves against NHS Digital information standards. |
| Department of Health and Social Care | DHSC | A department of the Government with responsibility for government policy for health and social care matters and for the NHS in England along with a few elements of the same matters which are not otherwise devolved to the Scottish, Welsh or Northern Irish governments. |
| Disability Real Action Group of Norfolk | D.R.A.G.O.NS | A group of young people with disabilities that are looking to make sure that SEND opportunities, in Norfolk, are accessible and that young people are enjoying their services. |
| Duty of Candour | DoC | Regulation 20 of the Health and Social Care Act 2012 (Regulated Activities) Regulations 2014 to ensure that providers are open and transparent with people who use services or their representatives. |
| East of England Ambulance Service NHS Trust | EEAST | Ambulance service which operates in the East of England. |
| EasyRead | - | An accessible format which can be used by people with learning difficulties. |
| Electrocardiography | ECG | An ECG is a test used to measure the electrical activity of the heart. |
| Electronic patient care record | ePCR | A patient care record which is in electronic format. |
| Emergency operations centre | EOC | Control centre for managing call receipt, triage and dispatch functions. |
| Face arm speech time | FAST | A simple test to help people recognise the signs of stroke and understand the importance of emergency treatment |
| Freedom to Speak Up | FTSU | A national initiative to apply measures to enable staff to speak out about patient safety and other concerns confidentially or anonymously. |
| Friends and Family Test | FFT | A feedback tool that anyone can use to give quick, anonymous feedback to providers of NHS services. |
| General practitioner | GP | A medical practitioner who treats acute and chronic illnesses and provides preventive care and health education to patients. |
| Glasgow Coma Scale | GCS | A clinical scale used to reliably measure a person's level of consciousness. |
| Glyceryl trinitrate | GTN | Drug for heart disease patients to dilate the blood vessels. Delivered as a spray or in tablet form. |
| Hazardous Area Response Team | HART | Specialist ambulance unit that provides medical care to patients in hazardous or ‘hot’ environments. They utilise special vehicles and equipment. |
| Health and Social Care Act | HSCA | An Act of the Parliament of the United Kingdom. It provides for the most extensive reorganisation of the structure of the National Health Service in England to date. It removed responsibility for the health of citizens from the Secretary of State for Health, which the post had carried since the inception of the NHS in 1948. |
| Health overview and scrutiny committee | HOSC | Provides external assessment of any NHS consultation process giving local assurance that the business cases for any future NHS developments are robust. |
| Healthcare Quality Improvement Partnership | HQIP | An independent organisation to promote quality in healthcare, and in particular to increase the impact that clinical audit has on healthcare quality improvement. |
| Healthwatch | An independent national body with the power to monitor the NHS and to refer patients’ concerns to a wide range of authorities. It represents the interests of patients as consumers, strategic commissioning, pursues and refers patient complaints and contributes to national public debate on the NHS. | |
| Hear and treat | - | Over-the-telephone advice that callers who do not have serious or life-threatening conditions receive from an ambulance service after calling 999. |
| Information Governance Group | IGG | A group within EEAST in place to ensure that all information systems and processes comply with the Data Protection Act. |
| Integrated Care Board | ICB | NHS organisations set up with responsibility to organise and oversee the delivery of NHS and social care services in England. |
| Integrated Care System | ICS | Partnerships between the organisations that meet health and care needs across an area, to coordinate services and to plan in a way that improves population health and reduces inequalities between different groups. |
| Integrated Performance Report | IPR | Dashboard used within EEAST that provides information against set key metrics. |
| Joint Royal College Ambulance Liaison Committee | JRCALC | Expert committee responsible for the production of clinical guidelines for ambulance services in the UK |
| Key performance indicator | KPI | Clear, comparative gauge for ICBs, boards, local authorities, patients and the public to monitor about the quality of health services commissioned by ICBs and the associated health outcomes. |
| Learning from Deaths | LfD | National guidance for NHS trusts on working with bereaved families and carers. It advises trusts on how they should support, communicate and engage with families following a death of someone in their care. |
| Learning From Patient Safety Events | LFPSE | A national NHS service for the recording and analysis of patient safety events that occur in healthcare. |
| Local authority | - | An organisation that is officially responsible for all the public services and facilities in a particular area. |
| Mean | - | A number that is the average of a set of numbers |
| Median | - | The middle value when a range of values is arranged in order. |
| Mental Capacity Assessment | MCA | An assessment undertaken by healthcare professionals to determine if the individual is able to make a decision for themselves. |
| Metrics | - | Set of ways of quantitatively and periodically measuring performance. |
| Myocardial infarction | MI | Clinical term for a heart attack. |
| National Guardian’s Office | NGO | The organisation who works to make speaking up become business as usual to effect cultural change in the NHS. |
| National Health Service | NHS | The publicly funded healthcare system of England. It is the largest and the oldest single-payer healthcare system in the world. |
| National Institute for Health Research | NIHR | Organisation that funds health and care research in the United Kingdom. |
| National Patient Safety Alert | NPSA | Issued by NHS Improvement to rapidly warn the healthcare system of risks |
| National Performance Advisory Group | NPAG | Self funding NHS organisation that provides a number of services to support NHS organisations |
| National Quality Board | NQB | Provides advice, recommendations and endorsement on matters relating to quality, and acts as a collective to influence, drive and ensure system alignment of quality programmes and initiatives. |
| National Reporting and Learning Service | NRLS | A central database of patient safety incident reports. |
| National staff survey | - | A way of ensuring that the views of staff working in the NHS inform local improvements and input in to local and national assessments of quality, safety, and delivery of the NHS Constitution. |
| Never Events | - | Incidents that required investigation under the previous Serious Incident framework |
| NHS Digital | NHSD | The national information and technology partner to the health and care system. |
| NHS England | NHSE&I | The lead body for the National Health Service in England. |
| Non-Emergency Patient Transport Service | NEPTS | Provides transport to and from premises providing NHS healthcare and between NHS healthcare providers. This is also known as scheduled transport or non-emergency service. |
| Norfolk and Norwich SEND Association | NANSA | A registered charity dedicated to improving the lives of people in Norfolk with disabilities and special educational needs. |
| Outcome from out-of-Hospital-Cardiac Arrest | OHCA | A prospective study, collecting information on all out-of-hospital cardiac arrests in the UK. |
| Oxygen saturation | SpO2 | Term referring to the fraction of oxygen within the haemoglobin levels. A normal level would range between 95-97%. |
| Pandemic | - | A disease that exists in almost all of an area or in almost all of a group of people. |
| Paramedic | - | A registered healthcare professional, working predominantly in the pre-hospital and out-of-hospital environment. |
| Parliamentary and Health Service Ombudsman | PHSO | A legal organisation who make final decisions on complaints that have not been resolved by the NHS in England and UK government departments and other UK public organisations. |
| Patient Advice and Liaisons Service | PALS | PALS queries are processed by the Patient Services team who are the first point of contact for enquiries from the public or other healthcare organisations. |
| Patient and Public Involvement | PPI | The practice where people with health conditions (patients), carers and members of the public work together with organisations. |
| Patient care record | PCR | All NHS providers are required to record the care given to a patient on a patient care record. |
| Patient Facing Staff Hours | PFSH | A term used to describe resources available for patient care. |
| Patient Safety and Experience Group | PSEG | A group within EEAST in place to ensure that incidents and patient feedback are used to reduce risks and improve our services and patients’ experiences. |
| Patient safety incident | PSI | Any unintended or unexpected incident which could have (or did) lead to harm for one or more patients receiving NHS care. |
| Patient Safety Incident Response Framework | PSIRF | An NHS process to further improve patient safety. |
| Payment by results | - | The payment system in England under which commissioners pay healthcare providers for each patient seen or treated, taking into account the complexity of the patient’s healthcare needs. |
| Primary care | - | Out-of-hospital health services that play a central role in the local community. |
| Primary percutaneous coronary intervention | PPCI | Commonly known as coronary angioplasty or simply angioplasty, is a therapeutic procedure to treat the narrowed coronary arteries of the heart found in coronary heart disease. |
| Public Health England | PHE | An executive agency of the Department of Health and Social Care that exists to protect and improve the nation’s health and wellbeing. |
| Quality Governance Committee | QGC | An EEAST committee which has authority from the Trust Board to be assured that progress is being made on the assurance processes for clinical effectiveness, patient safety and patient experience. |
| Quarter 1 (2,3,4) | Q1 (2,3,4) | Financial year (1st April – 31st March) quarter indicator. |
| Research Ethics Committee | REC | Responsible for the ethical conduct of research studies designed to increase understanding of workplace factors that contribute to ill-health and workplace accidents. |
| Return of spontaneous circulation | ROSC | The resumption of sustained perfusing cardiac activity associated with significant respiratory effort after cardiac arrest. |
| Scheduled transport service | STS | A non-emergency service provided to patients who are unable to convey themselves for outpatients’ appointments. This is also sometimes known as Patient Transport Service or non-emergency service. |
| See and treat | - | Patients who are treated at home by ambulance staff and do not require taking to a hospital or other care centre |
| Serious Incident | SI | An event or circumstance that could have resulted, or did result, in unnecessary damage, loss or harm such as physical or mental injury to a patient, staff, visitors or members of the public. |
| Service user | Anyone who uses, requests, applies for or benefits from health or local authority services. | |
| Short Message/Messaging Service | SMS | A text messaging service within most telephone, Internet and mobile device systems. |
| Special Educational Need and/or Disability | SEND | A term used if a child or young person has a significantly greater difficulty in learning that the majority of others of the same age or has a disability which prevents or hinders them from making use of educational facilities of a kind generally provided for others of the same age in mainstream schools or mainstream post-16 institutions |
| Stakeholders | - | Anyone with an interest in the way services are delivered including service users, carers, patients, service providers, staff, health professionals and partner organisations, councils and other community or voluntary groups. |
| ST-elevation myocardial infarction | STEMI | A heart attack recognised by characteristics on an ECG. |
| STEMI care bundle | - | A set of interventions that when used together significantly improve patient outcomes for a heart attack. |
| Strategy | - | A plan of action designed to achieve a long-term or overall aim. |
| Stroke | TIA | A stroke happens when the blood supply to the brain is disturbed. |
| Stroke diagnostic bundle | SCB | A set of assessments that when applied provide information indicating as to whether a stroke has occurred. |
| Structured Judgement Reviews | SJR | Method for undertaking a clinical review of care for adults as part of the NHS learning from deaths programme |
| Summary Care Record | SCR | An electronic record of important patient information, created from GP medical records which can be seen and used by authorised staff in other areas of the health and care system involved in the patient's direct care. |
| Time for Me App | A personal wellbeing tool to help our staff and volunteers focus on their own personal happiness and life progress. | |
| United Kingdom | UK | The United Kingdom is the official name for the country consisting of Great Britain and Northern Ireland. |
| Unscheduled Care Coordination Hub | UCCH | A scheme that is designed to provide timely access to urgent care in the community for patients with immediate care needs. |
| Utstein | - | The Utstein Style is a set of guidelines for uniform reporting of cardiac arrest. The Utstein Style was first proposed for emergency medical services in 1991. |
