EEAST Infection Prevention & Control 2024-25 Annual Report
Date published: 14 October 2025
Summary
This Annual Infection Prevention and Control (IPC) report fulfils our statutory duty under the Health and Social Care Act 2008 (IPC Code of Practice). It covers the Trust’s IPC performance between April 2024 and March 2025. Date of Report: July 2025 Author: Shaun Watkins – Head of Infection Prevention and Control
In this report
- Executive Summary
- Introduction and Trust commitment to IPC
- About this report
- IPC Code of Practice – 10 Compliance Criteria (Summary)
- Celebrating Our Achievements in Infection Prevention and Control (2024-2025)
- Trust IPC Infrastructure
- IPC Governance structure
- Audit Programme and Compliance Monitoring
- Audit outcomes for 2024-2025
- Compliance audit summary
- Make Ready Service
- Infectious Disease Preparedness and Response
- Occupational Exposure Incidents 2024-2025
- Antimicrobial stewardship
- Occupational health
- Training
- 2025-2026 Objectives
- Head of IPC Summary
Executive Summary
This report reviews the East of England Ambulance Service NHS Trust’s infection prevention and control (IPC) performance from April 2024 to March 2025. The Trust remains committed to protecting patients and staff through strong IPC governance, thorough auditing, and ongoing staff training.
Key achievements include building a dedicated IPC team, improving station and uniform compliance, enhancing cleaning standards, and effectively managing emerging infectious threats like measles and mpox. Occupational exposure incidents rose, partly due to better reporting and increased disease cases, supported by a new in-house Occupational Health service.
Challenges with vehicle cleaning and premises cleaning contractor transitions were addressed through restructuring and collaboration with the Make Ready team and facilities manager.
Looking ahead, priorities include improving cleaning compliance, waste management, staff audit quality, and IPC training to ensure continued protection and safety.
Introduction and Trust commitment to IPC
Our Trust places infection prevention and control at the core of both clinical excellence and operational management. We are fully committed to allocating the necessary resources to protect our patients, their families, staff, and the wider community effectively. This commitment is reflected in our ongoing focus on preventing healthcare-associated infections and continuously enhancing the hygiene standards of our vehicles, stations, and staff practices.
Key areas the Trust prioritizes include:
- Monitoring the number and types of clinical procedures performed across the Trust, alongside robust systems that support infection control and thorough decontamination.
- Supporting all staff activities that contribute to the prevention and control of infection within our service.
- Maintaining and regularly updating comprehensive policies on infection prevention, control, and decontamination.
- Delivering ongoing education and training programs to ensure our teams are equipped with the latest knowledge and best practices.
- Establishing clear accountability frameworks to reinforce responsibility for infection prevention and control at all levels.
- Utilising expert infection prevention advice to guide our strategies.
- Embedding infection prevention and control principles seamlessly into all aspects of service delivery, development, and innovation.
This report outlines our progress, challenges, and ongoing initiatives to uphold the highest standards of infection prevention and control across our ambulance service.
About this report
This Annual Infection Prevention and Control report fulfils our statutory duty under the Health and Social Care Act 2008 (IPC Code of Practice). It covers the Trust’s IPC performance between April 2024 and March 2025.
The report assures the Trust Board, regulators, and the public that we have effective systems in place to prevent and manage infection risks. It also demonstrates compliance with the IPC Code’s 10 criteria, including governance, cleanliness, antimicrobial stewardship, staff training, risk management, and occupational health.
Key sections include:
- IPC team structure and leadership.
- Progress against 2024–25 IPC objectives.
- Monitoring methods such as audits and inspections.
- Goals for 2025–2026 based on national guidance and service needs.
IPC Code of Practice – 10 Compliance Criteria (Summary)
- IPC systems and oversight: Defined responsibilities and management structures.
- Clean environments: High cleaning standards for stations, vehicles, and equipment.
- Antimicrobial stewardship: Promoting responsible use of antibiotics.
- Information sharing: Timely and clear communication to staff and patients.
- Identification and response: Early detection and management of infections.
- Staff training: Up-to-date IPC education for all employees.
- Isolation procedures: Effective PPE use and patient handover alerts.
- Lab support: Access to microbiological advice via NHS partners.
- Policies and protocols: Reviewed and implemented IPC policies.
- Occupational health: Support for staff health and safety, including vaccinations and post-exposure care.
Celebrating Our Achievements in Infection Prevention and Control (2024-2025)
The 2024–2025 reporting year has been a period of significant progress and achievement for the East of England Ambulance Service NHS Trust’s Infection Prevention and Control (IPC) team. We have strengthened our infrastructure, enhanced collaboration, and driven improvements that directly contribute to safer environments for our patients, staff, and communities.
Key milestones include:
- Fully Established IPC Team: We are proud to have built a strong and dedicated IPC team with clear roles and expertise. This foundation enables us to respond swiftly and effectively to infection prevention challenges across the Trust.
- Training of Compliance Audit Facilitators (CAFs): Targeted IPC training has empowered CAFs, enhancing knowledge and capability, which is essential in embedding infection control practices within everyday operations.
- Improvements in Uniform and Station Compliance: We have seen tangible improvements in uniform and station compliance, reflecting a culture of accountability and attention to detail at all levels.
- Co-Joined Working with Estates: Collaborating closely with the Estates team, specifically the facilities manager, has led to coordinated efforts in maintaining and enhancing the physical environment, ensuring our stations meet the highest standards of cleanliness and infection prevention.
- Implementation of New Contract Cleaning Compliance: By overseeing rigorous contract cleaning standards, we have ensured that external cleaning services deliver improved quality of cleaning standards.
- Introduction of Offensive Waste Streams and exceeding NHS Compliance Targets: We successfully introduced offensive waste streams, not only meeting but exceeding national NHS targets, demonstrating our commitment to responsible and safe waste management.
- Collaborative audits have increased in number, allowing for more comprehensive and transparent assessment of IPC standards across all operational areas. This has resulted in improved consistency in audits which now demonstrate the highest quality and consistency of data ever recorded, enabling better insight and more targeted improvement actions.
- IPC Auditors Undertaking Diplomas in IPC: Several IPC auditors are now pursuing advanced IPC qualifications, reflecting our commitment to professional development and raising standards through expert knowledge.
- IPC Practitioner Passed Postgraduate Certificate in IPC: Congratulations to our IPC practitioner for successfully completing a Postgraduate Certificate in Infection Prevention and Control, a significant achievement that brings further advanced expertise into the team.
- Review and Alignment of Audits with Cleaning Standards: The IPC team has thoroughly reviewed audit tools and protocols to align with updated cleaning standards, ensuring that monitoring remains relevant, rigorous, and actionable.
- Effective Response to Emerging Threats: The IPC team has proactively responded to cases of MPOX (monkeypox) and measles, managing prevalence with swift action and clear communication, ensuring ongoing protection for staff and patients.
These accomplishments highlight our dedication to excellence in infection prevention and control. They set a strong foundation for continued progress and innovation in the coming year, as we strive to protect everyone who relies on our services.
Trust IPC Infrastructure
At EEAST, infection prevention and control (IPC) is a shared responsibility across all levels of the organisation, from frontline staff to the Trust Board. The dedicated IPC Team leads on specialist advice, guidance, and monitoring to support safe, effective care.
EEAST’s IPC Structure:
- All staff: Shared responsibility for reducing infection risks.
- Dedicated IPC Team: Provides specialist advice, oversight, and monitoring.
IPC Team Composition:
- Director of IPC: Chief Paramedic/AHP & Director of Quality — Executive lead for clinical quality and safety
- Head of IPC (Deputy DIPC): Master’s educated, 14+ years IPC experience, 5 years in post.
- IPC Practitioner: Experienced EMT with postgraduate IPC qualification
- 3 IPC Auditors: Former clinicians — 2 undertaking IPC Diploma Level 3, 1 due to begin.
Collaborative Partnerships:
- Facilities Manager: Leads on waste management and cleaning contractor implementation.
- Liaison with: o Clinicians o Directorate and operational managers o Estates and Facilities o Clinical Governance o Risk and Health & Safety o Occupational Health o Procurement and Medical Devices
IPC Governance structure
- Top-Level Governance:
- Quality Governance Committee
- Compliance and Risk Group
- IPC Group (Principal forum for senior-level IPC discussion and decisions)
- IPC Group Details:
- Chaired by Deputy Director of Infection Prevention and Control (Deputy DIPC)
- Meets bi-monthly.
- Multi-disciplinary (includes representatives from interested directorates and senior management)
- Responsibilities: -- Agree and review IPC policies. -- Assess risk profiles. -- Oversee mitigation actions.
- Subsidiary Groups Feeding into IPC Group:
- Several subsidiary groups to IPC Group
- Supported by IPC members for alignment and shared accountability.
- Operational Engagement:
- IPC Practitioner and IPC Auditors regularly attend: -- Operational Delivery Group (ODG) meetings (within each sector) -- Purpose: --- Share best practices. --- Highlight improvement areas. --- Communicate IPC policy updates. -- Strengthen connection between IPC leadership and frontline services.
Audit Programme and Compliance Monitoring
The Trust operates a comprehensive audit programme that is reviewed annually to maintain relevance and effectiveness. It covers emergency and non-emergency vehicles, operational stations, call centres, staff uniform, and overall compliance with infection prevention and control (IPC) procedures.
A tiered audit structure supports robust monitoring:
Local Managerial Audits – Conducted by frontline managers for day-to-day compliance. Quality Assurance Audits – Carried out by the IPC team to validate standards and provide oversight. External Audits – Undertaken by the Community Engagement Group to offer independent assurance.
Audits are recorded through a live online platform, enabling real-time monitoring, trend analysis, photographic evidence capture, and action tracking to close audit loops efficiently.
Operational patient facing vehicles.
Vehicles undergo:
- 12-week service cleans (full vehicle)
- 48-hour interim cleans (Patient treatment area, cab and exterior)
Audits assess:
- Cleanliness of the cab, saloon, and exterior
- PPE availability
- Equipment cleanliness and readiness
Station and Call Centre Audits
Stations are audited monthly with a compliance threshold of 85%, aiming for 95%. Audits focus on:
- Medical equipment storage
- Cleanliness standards
- IPC signage
- Waste, sharps, and linen management.
- Kitchens, toilets, and dirty utility areas
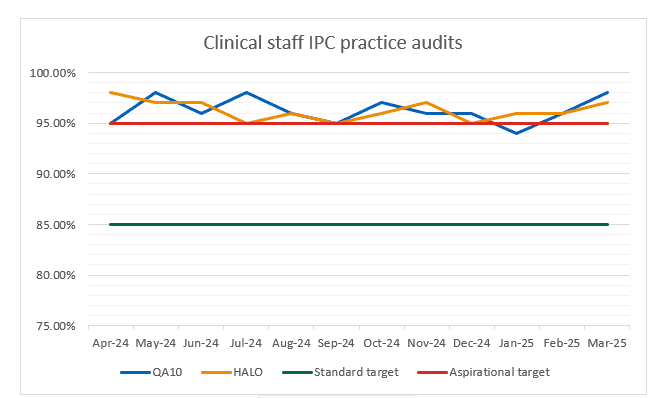
Staff IPC Compliance Audits
Three audit types assess staff compliance:
-
Uniform Audits – Monitoring adherence to ‘bare below the elbows and uniform standards to support hand hygiene.
-
QA10 Audits – Observations during clinical ride-outs, focusing on PPE use, hand hygiene, waste disposal, and equipment decontamination.
-
HALO Audits – Conducted during hospital handovers, reviewing IPC practice at the interface of care.
These audits underpin the Trust’s IPC assurance framework, support improvement actions, and help drive a culture of accountability and high standards in infection prevention.
Audit outcomes for 2024-2025
Chart 1: Operational stations compliance
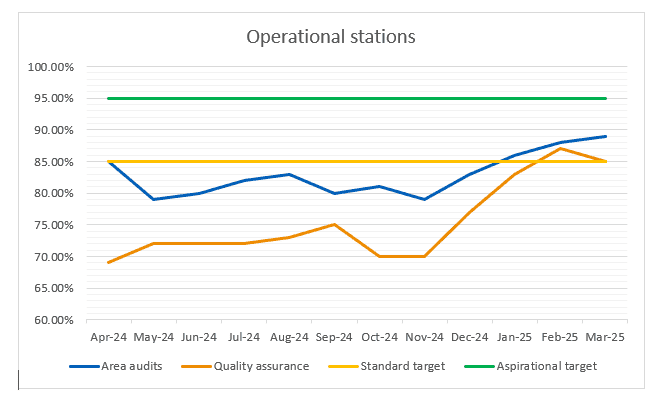
Chart 2: Patient facing vehicles
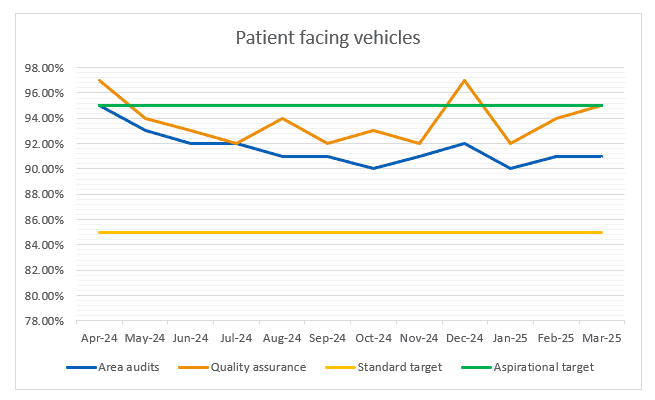
Chart 3: Vehicle cleaning schedule compliance
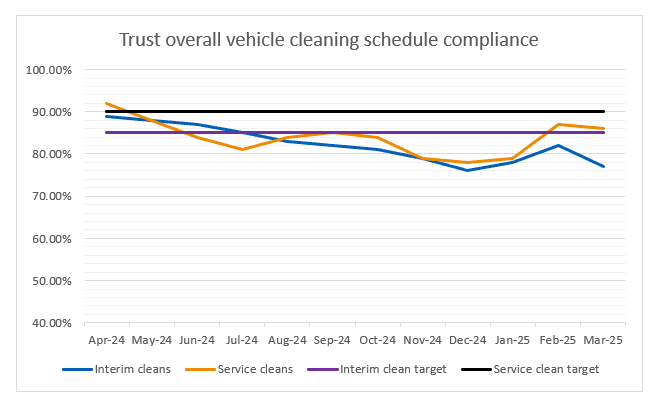
*Refer to the Make ready section below for detail on vehicle cleaning compliance
Chart 4: Clinical staff uniform
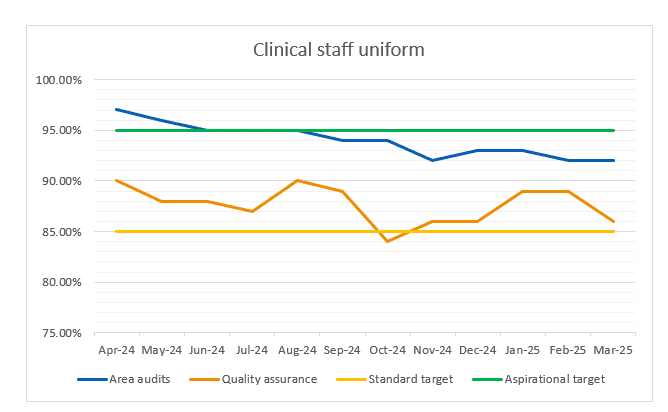
Chart 5: Clinical IPC practice audits
Compliance audit summary
Between April 2024 and March 2025, the Trust experienced steady progress across infection prevention and control (IPC) audit areas. A highly accurate correlation between local area audits and quality assurance scores developed throughout this reporting period following implementation and training of local compliance auditors.
For stations, the period included the procurement of a new cleaning contractor, which caused fluctuations in compliance due to the transition. Additionally, local management of clinical waste and some housekeeping issues were identified as barriers to achieving higher scores. Despite these challenges, improvements were evident, with local audits effectively reflecting true quality standards.
In vehicles, there was a slight overall decline in compliance, primarily driven by reduced vehicle cleaning standards. This issue is explored further in the Make Ready section of the report, highlighting the causes and resolutions to the vehicle cleaning compliance.
Uniform compliance showed a different trend. Although uniform standards appeared lower compared to the previous year, this was largely due to a focused campaign on “bare below the elbows” and enhanced management processes, which improved local audit accuracy. While local audits showed a dip, quality assurance demonstrated some improvement in bare below the elbows compliance and narrowed the gap between local and quality scores. Overall, uniform standards are met, but there remains room for continued improvement.
Staff observation audits, conducted by local managers, consistently recorded high compliance with good staff practice. However, elements such as waste disposal and PPE use have been flagged through other channels as areas needing improvement. The Head of IPC has set objectives to tighten assurance around the quality of staff observation auditing and enhance clinical practices, ensuring sustained IPC excellence moving forward.
Make Ready Service
Our Make Ready Service continues to play a critical role in ensuring that all frontline vehicles are prepared, safe, and compliant for operational use. Throughout 2023–2024, Make Ready teams across EEAST consistently delivered high standards in vehicle preparation, including the cleaning, stocking, and servicing of equipment and consumables.
During 2024–2025 the Make Ready function experienced a number of changes. The service’s budget was adjusted to align with the organisation’s strategic financial planning, resulting in staffing and fleet availability pressures, alongside increased operational demand. These challenges contributed to some fluctuations in vehicle cleaning compliance in certain areas.
In the latter part of the year, a new Head of Make Ready was appointed, and a comprehensive service restructure was initiated. This restructure has focused on aligning the Make Ready model to the new budget, operational needs, and the future requirements of the service. The IPC team has worked closely with Make Ready leadership throughout this period, supporting workforce planning and the recruitment of key managerial roles to ensure a resilient and effective service moving forward.
Although some variability in compliance has been observed during this transitional phase, the new working models and strengthened leadership structure are expected to deliver greater consistency and improved compliance in 2025–2026. These developments provide increased assurance to IPC and reinforce our continued commitment to delivering clean, safe, and operationally ready vehicles for our patients and crews.
To add, as this report has been produced following year end, a significant improvement regarding vehicle cleaning compliance has been recorded in all areas that were previously below target. This will be captured in the following years report.
Infectious Disease Preparedness and Response
Over the past year, the IPC team has swiftly responded to several infectious disease threats to protect staff and maintain safe patient care.
Lassa Fever Preparedness
Lassa fever is a viral hemorrhagic illness endemic in West Africa with potential for severe outbreaks. In early 2025, after a UKHSA alert on Lassa fever, the IPC team quickly developed communications and a system wide process for managing suspected cases. This included enhanced PPE guidance, isolation protocols, and triggers to involve Hazardous Area Response Teams (HART). The prompt activation of these measures demonstrated effective frontline protection.
Mpox Preparedness
Mpox, caused by an orthopoxvirus related to smallpox, has seen recent outbreaks in multiple regions. Following Mpox Clade 2’s emergence and increased Clade 1 cases, IPC adapted protocols after its HCID status was downgraded. Updated PPE, isolation, and referral procedures were communicated clearly. Staff effectively followed protocols and escalated cases when needed, confirming service readiness.
Measles Preparedness
Measles is a highly contagious viral illness that remains a significant public health concern due to outbreaks and complications. With over 1,200 UK measles cases reported, the IPC team used incident reporting and worked with health protection teams to manage staff exposures. Immediate guidance and joint risk assessments with occupational health ensured staff were protected by verified vaccinations, even when PPE was not worn. Across all incidents, the IPC team’s timely communication, clear protocols, collaboration, and risk assessments ensured staff safety and operational resilience, maintaining readiness for emerging infection risks.
Occupational Exposure Incidents 2024-2025
The Trust records incidents through the online reporting system, Datix to ensure ease of access staff can submit incident reports either online or via a single point of contact phone number. Where an incident occurs, the protocol is to follow immediate safety actions and then refer to A&E/OH for risk assessment to determine any necessary treatment or prophylaxis. The IPC related incidents are split into three main categories and are reported on through the monthly IPC report, they area classed as:
- Occupational exposure incidents
- Contaminated needle stick injuries
- Splashes of blood or bodily fluids to mucous membranes
Table 1: Quantity of incidents by type
| Total incidents reported | Contaminated sharps | Splash incidents | Potential exposure | |
|---|---|---|---|---|
| Apr | 11 | 4 | 3 | 4 |
| May | 16 | 5 | 7 | 4 |
| Jun | 10 | 4 | 3 | 3 |
| Jul | 15 | 6 | 5 | 4 |
| Aug | 10 | 5 | 4 | 1 |
| Sep | 9 | 3 | 4 | 2 |
| Oct | 11 | 8 | 2 | 1 |
| Nov | 0 | 0 | 0 | 0 |
| Dec | 13 | 6 | 4 | 3 |
| Jan | 2 | 2 | 0 | 0 |
| Feb | 6 | 3 | 1 | 2 |
| Mar | 6 | 3 | 3 | 0 |
| Total incidents: | 109 |
This year saw a rise in reported incidents, increasing from 76 to 109. While this reflects a higher number of exposures, it also indicates improved awareness and reporting, supported by ongoing communication from the IPC and Occupational Health teams. Staff are encouraged to report incidents promptly, enabling timely treatment and shared learning.
The increase partly reflects higher cases of measles and mpox, with clear protocols in place to guide staff response. These helped ensure early recognition and appropriate use of PPE.
The introduction of an in-house Occupational Health team has streamlined follow-up care, including quicker access to post-exposure bloods and support.
Key learning from this year includes the need for better sharps management and more proactive PPE use, particularly in situations involving splash or spitting risk. These particular elements will align with this coming years IPC objectives.
Antimicrobial stewardship
The Trust maintains a strong antimicrobial stewardship (AMS) framework to optimize patient outcomes and reduce resistance risks. Governance is clearly defined, with oversight by the Clinical Practice and Medicines Governance groups, aligned with national guidelines like JRCALC and CQC Regulation 12.
The Medicines Management Group reports regularly to the Quality Governance Committee. The Trust has an executive AMS lead who monitors antimicrobial use. AMS activities are benchmarked against local and primary care guidance.
Prescribing is audited and supported by mandatory national training. While currently binary, plans are in place to introduce electronic prescribing. Prescribing data is tracked through the electronic patient care record (EPCR), with increasing audit frequency and improved reporting.
Resources like JRCALC guidance support all staff, ensuring ongoing AMS quality improvement.
Occupational health
During this period, the Trust shifted from an outsourced to an in-house occupational health (OH) service, improving integration, responsiveness, and collaboration, especially with infection prevention and control (IPC).
OH is crucial for protecting staff health and reducing infection risk, ensuring assessments and vaccinations, including hepatitis B, MMR, varicella, and flu, follow national Green Book guidance.
IPC and OH teams work closely on exposure incidents, providing timely assessments, post-exposure prophylaxis, and follow-up care to ensure staff safety and operational continuity.
The IPC team also supports OH in delivering the annual flu vaccination campaign, using joint planning and peer vaccinators to maximise uptake and reduce staff absence during winter.
Bringing OH in house has enhanced our ability to respond to staff health needs and deliver coordinated infection control, reinforcing a culture of safety and prevention.
Training
At EEAST, Infection Prevention and Control (IPC) training is essential. All personnel are required to complete Statutory and Mandatory (StatMan) training, aligned with the national Core Skills Training Framework (CSTF), ensuring high standards and consistency across the sector. >90% compliance was achieved during 2024–2025.
Our Trust maintains high compliance with IPC StatMan training, and all new staff receive induction training developed specifically by the Head of IPC. This training is tailored to the unique operational context of ambulance services, offering practical, relevant knowledge from the outset.
This year, IPC training delivery and the development utilising the NHSE IPC Education Framework are key objectives. These initiatives aim to enhance the quality, relevance, and reach of IPC education across the Trust, supporting continuous improvement and embedding a strong infection prevention culture throughout the organisation.
2025-2026 Objectives
Upcoming Priorities for 2025
As we look forward to 2025, the Infection Prevention and Control (IPC) team will focus on a series of targeted objectives aimed at strengthening standards, embedding best practice, and enhancing staff knowledge across the ambulance service. These priorities are aligned with internal audit findings, national policy, and learning from incidents, ensuring that infection prevention remains central to the Trust’s operational and clinical delivery.
1. Vehicle Cleaning Compliance Continued collaboration with Make Ready teams will support improvements in vehicle cleanliness through targeted training, recruitment, and regular performance monitoring. Measured by: Monthly vehicle audits, weekly cleaning metrics, IPC audits, and CQC feedback.
2. Station Cleaning Standards Joint audits and data reviews will address variability and ensure consistent standards, benchmarked against NHS Cleaning Standards 2025. Measured by: Station audit scores, monthly compliance reports, and contractor performance reviews.
3. Clinical Waste Management Targeted communications and training will reduce waste disposal errors and improve compliance, supported by site visits and incident monitoring. Measured by: Reduction in clinical waste incidents, audit results, and training compliance rates (Waste 92%, IPC >90%).
4. Staff Observation Audits Audit quality and consistency will be enhanced through training and a new quality assurance model, developed with the training school. Measured by: Increased audit submissions, quality assurance feedback, and assessor competency reviews.
5. Staff Practice in PPE, Hygiene, and Uniform Audit data will guide further training and communications to improve consistent PPE use, hand hygiene, and uniform standards. Measured by: Improved audit compliance, reduced IPC breaches, and staff feedback.
6. IPC Education Enhancements Training content will be updated to better reflect ambulance service needs, enhancing induction and aligning with national frameworks. Measured by: Training delivery outcomes, knowledge assessments, and improvements in related audits.
7. IPC Team Development Professional development, audit accuracy, and appraisal processes will ensure the team is skilled and ready for future challenges. Measured by: Completion of training, audit quality metrics, appraisal records, and staff engagement.
Head of IPC Summary
This year has been one of continued progress for Infection Prevention and Control (IPC) at EEAST. Building on strong foundations, we’ve strengthened our governance, enhanced audit consistency, and responded swiftly to rising infectious disease risks, including national increases in measles and mpox.
Incident reporting rose from 76 to 109, driven by improved awareness and stronger collaboration between the IPC and Occupational Health teams. The introduction of our in-house Occupational Health service has significantly improved the speed and quality of post-exposure care and staff support.
Audit programmes saw greater alignment to national standards, supported by trained Compliance Audit Facilitators and improved local validation. While some fluctuations were noted in vehicle and station compliance during contractor transitions, these were met with targeted action and reinforced by strengthened Make Ready leadership.
We’ve also made strong progress in staff practice, particularly around “bare below the elbows” compliance and translating learning from incidents into practical changes. Our new waste streams and audit reviews demonstrate a clear commitment to both environmental and clinical standards.
Looking ahead to 2025–2026, our objectives focus on improving cleaning compliance, enhancing clinical waste management, increasing the quality of staff audits, and tailoring training to better reflect ambulance service needs. With a developing IPC team, we remain committed to maintaining a safe, responsive, and learning-focused infection control environment.
Reducing the risk of infection transmission is fundamental to patient care, not only on an individual basis but also affecting the wider health economy. The strength of our successes this coming year will be demonstrated with greater integration of our learning and IPC practices becoming intrinsic to all elements of care episodes.
